Let These Pointers Lead You To Pleural Effusion Reporting Perfection
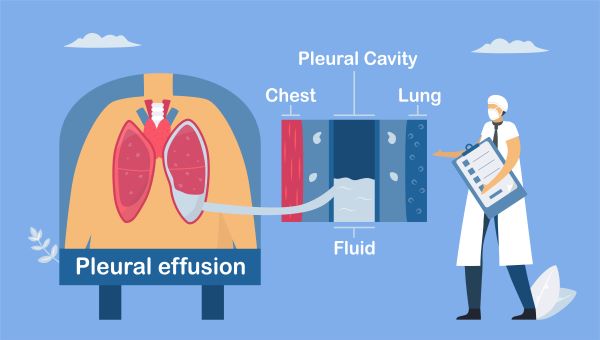
Hint: The Code first notes are crucial reading. Thin membranes, known as pleura, cover the outside of the lungs and the inside of the chest cavity, and sometimes, too much fluid accumulates within this lining, causing respiratory problems. Anesthesiologists often have a hand in the management and/or treatment of patients with pleural effusion, so be ready to report the condition as accurately as possible. Read on for helpful guidance on how to navigate the provider’s documentation and assign and sequence ICD-10-CM codes correctly for these cases. Understand This Condition Pleural effusion, sometimes referred to as “water on the lung,” is the build-up of excess fluid in the pleural space. There’s always a small amount of liquid between the two layers of the pleural membrane to help lubricate the lungs as they expand within the chest during breathing. However, if too much fluid builds up due to over-production or decreased lymphatic absorption, for example, problems can arise. The ICD-10-CM code set features three codes designated for pleural effusion diagnoses: While some people with pleural effusion have no symptoms, the fluid buildup may cause shortness of breath (dyspnea), rapid breathing (tachypnea), chest pain, cough, and fever. Various conditions, such as pneumonia, kidney disease, cirrhosis, or cancer, can lead to pleural effusion, but congestive heart failure (CHF) is the most common cause. Master Malignant Pleural Effusion Coding Code J91.0 is reserved to report a malignant pleural effusion (MPE) diagnosis — the provider determines that a malignancy is causing the pleural effusion. “MPE is an accumulation of cancer cells and fluid in the pleural space. The cancer, which is typically a lung cancer or another type of cancer that has spread to the pleural space, causes the increase in the pleural fluid,” says Carol Pohlig, BSN, RN, CPC, manager of coding and education in the department of medicine at the Hospital of the University of Pennsylvania in Philadelphia. Code first: Before you assign J91.0 for an MPE diagnosis and move on with your day, you’ll want to take a pause. Code J91.0 features a Code first note instructing you to report the underlying neoplasm as the first-listed diagnosis. Scenario: A patient is diagnosed with MPE caused by a malignant neoplasm of the main bronchus around the right hilum. In this case, you’ll assign C34.01 (Malignant neoplasm of right main bronchus) as the first code and then J91.0 as the second code. In this scenario, the provider determined the bronchial neoplasm was causing the patient’s MPE, but can you report MPE if the patient is diagnosed with any cancer? No, because the MPE must be the result of a specific malignancy. “Just because the patient has cancer and a pleural effusion at the same time, does not necessarily mean that the cancer is causing MPE. While an MPE is likely for a patient with lung cancer, it isn’t likely for a patient who may have testicular cancer in situ but also has acute on chronic CHF. In that case, the heart failure is more likely causing the effusion,” Pohlig explains. So, when coding MPE diagnoses, remember that documentation is your friend. If the provider diagnosed the patient with MPE in the medical record, look for information to support the diagnosis and what neoplasm is the underlying cause of the patient’s condition. However, a history of cancer doesn’t count when it comes to MPE. If a patient has a personal history of breast cancer but isn’t actively receiving treatment for the cancer, then the pleural effusion wouldn’t be considered malignant. Code the Underlying Condition First Not all pleural effusions are caused by malignancies. Non-malignant pleural effusion can be a result of a myriad of issues including cardiopulmonary (CHF, pulmonary embolism, pneumonia) and inflammatory (lupus, rheumatoid arthritis) conditions. In situations where the physician determines the cause of the patient’s pleural effusion, you’ll assign J91.8. While the cause of this pleural effusion won’t be cancer, you’ll use the same logic to report the condition. “Code J91.8 should be used for the non-malignant effusion, but the cause of the effusion must also be reported since this is a manifestation code,” Pohlig says. As a helpful reminder, the ICD-10-CM code set places a Code first note under J91.8 instructing you to assign a code for the underlying disease before J91.8. Scenario: The provider diagnoses a patient with pleural effusion caused by pneumonia due to Methicillin-resistant Staphylococcus aureus (MRSA). You’ll assign J15.212 (Pneumonia due to Methicillin resistant Staphylococcus aureus) first, followed by J91.8 to report the patient’s diagnoses. You may also encounter cases where the provider determines the patient’s pleural effusion is caused by non-respiratory conditions such as CHF or systemic lupus erythematosus (SLE). In those cases, you’ll refer to the Excludes2 note listed under parent code J91.- (Pleural effusion in conditions classified elsewhere). Typically, an Excludes2 note under the parent code indicates that the two conditions can be coded together. The Excludes2 note listed under J91.- allows you to report the pleural effusion and the non-respiratory condition together. “If the source causing the pleural effusion is non-respiratory, such as CHF or SLE, you would report this condition with the appropriate code listed within the corresponding code family,” Pohlig says. Bear in mind: Pleural effusion is commonly seen in patients with CHF. Typically, it’s minimal and is not specifically addressed other than by more aggressive treatment of the underlying heart failure. “In this situation, it should not be coded. However, it is acceptable to report pleural effusion (J91.8) as an additional diagnosis if the condition requires either therapeutic intervention or diagnostic testing,” per AHA Coding Clinic® (volume 2 number 2, 2015). However, the code for the Excludes2 listed condition may adequately represent both conditions and you will only need to report one code. For instance, if SLE is causing the patient’s pleural effusion, you’ll assign M32.13 (Lung involvement in systemic lupus erythematosus) since M32.13 also features “Pleural effusion due to systemic lupus erythematosus” as an additional descriptor. Rely on J90 for Pleural Effusion NOS Code J90 is reserved for cases where your provider may use other terms in their documentation to indicate a pleural effusion diagnosis of an undetermined origin. These terms are listed under J90 as synonyms: Code J90 features an Excludes1 note that prevents you from reporting the following conditions with J90 since the conditions listed below can’t exist together with J90: “Anesthesia coders do not usually receive more than just a simple explanation of the patient’s diagnosis as related to the anesthesia services provided. Fortunately, J90 allows coders to report pleural effusion NOS without having to request additional information, such as pathology or operative reports,” says Doris V. Branker, CHC, CPC, CIRCC, CPMA, CPC-I, CANPC, CEMC. Trust Your Instincts Regardless of whether you’ve been coding for years or are newly certified, you’ll set yourself up for coding success by carefully reviewing ICD-10-CM instructional notes and your provider’s documentation. And, as always, query the provider if you’re unsure of what’s causing the patient’s pleural effusion.