Follow These Tips to Clear Up COPD Diagnosis Coding

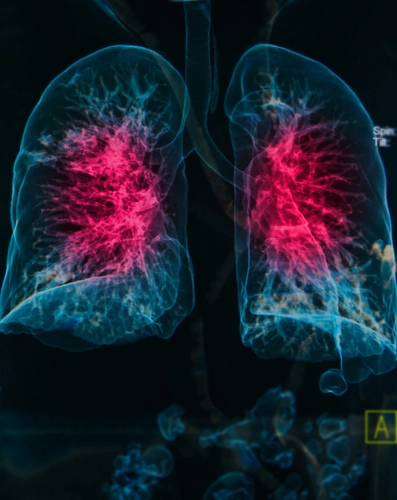
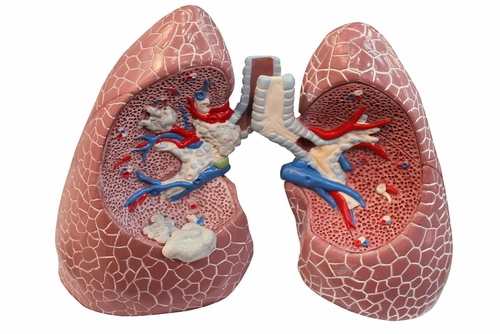
The use of anesthesia carries a lot of risk and can affect the patient's outcome, says Laureen Jandroep, CPC, COC, CPC-I, CPPM, founder/CEO Certification Coaching Organization, LLC in Oceanville, N.J. Physical status modifiers help paint a better picture of the encounter for the payer, as it clues the payer in to the patient's overall health at the time of anesthesia. Using P modifiers correctly can also support the use of certain diagnoses and document the level of expertise your anesthesia provider needed during a case. One example of this is COPD (chronic obstructive pulmonary disease) – which is why you need to be in-the-know about your options under ICD-10. Catch Up With This Quick Refresher "My concerns with coding COPD are the doctor not coding to the highest specificity," says Lisa Center, CPC, physician practice manager for Via Christi Hospital Pittsburg, Inc., in Pittsburg, KS. "We have been getting denials asking for more information. Our providers usually code 'unspecified,' so education has been key." Diagnosis codes for COPD allow for clear delineation of the disease as either an uncomplicated case or acute exacerbation. In other words, COPD is a condition for which clarity has improved in ICD-10-CM. "However, unless the patients' problem lists have been updated with the appropriate codes (rather than just cross-walked from ICD-9 codes), the specificity may have been lost," notes Carol Pohlig, BSN, RN, CPC, ACS, senior coding and education specialist at the Hospital of the University of Pennsylvania. Code family J44.- (Other chronic obstructive pulmonary disease) offers you the following code options: Terminology check: When the patient's condition is documented as an acute exacerbation, it is considered to be worsening, or is a decompensation of a chronic condition. Tip: When coding for COPD, be sure to review the notes in the Tabular List under "other chronic obstructive pulmonary diseases" (J44), to see what conditions fall under this heading, and for code also notes. For example, when reporting J44.0, remember to use an additional code to identify the infection. Also take note that J44.1 covers decompensated COPD, but excludes COPD with acute bronchitis. Moreover, J44.- requires you to code also the type of asthma, if applicable (J45.-) You may need to use additional code, such as Z77.22 (Contact with and [suspected] exposure to environmental tobacco smoke [acute] [chronic]).