Pin These Points for Precise Polyp Removal Coding
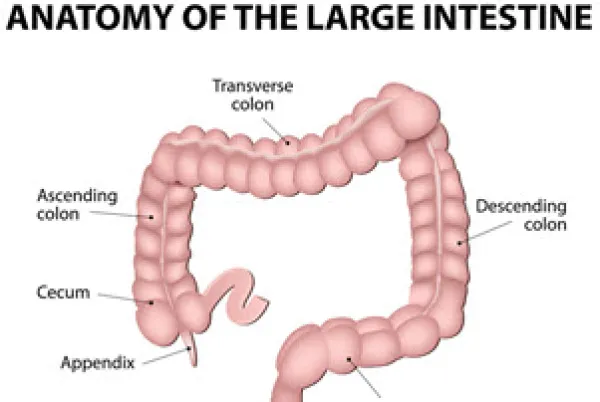
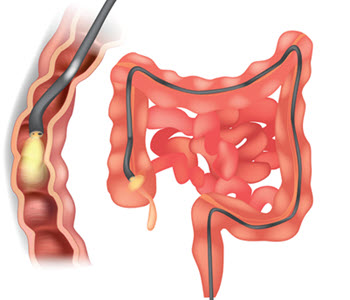
Check out this crash course in the anatomy of the colon. Polyps are something GI coders see constantly. Even so, it’s always a good time for a little refresher. Shore up your skills with help from this polyp coding primer. Identify Polyp Location When you code a polyp removal, knowing the specific location is essential to coding to the highest specificity. It’s not enough for the provider to just write “polyp in the rectal area” or “polyp higher in the colon.” ICD-10 codes are very location-specific for the colon region: You should use the non-specific polyp code D12.6 (Benign neoplasm of colon, unspecified) only as a last resort Anatomy refresh: The colon starts with the cecum in the lower right abdomen, and the appendix projects from the end. From the cecum, the colon then moves upward to the ascending colon. It then bends, running across the abdomen to the transverse colon before bending again toward the lower left abdomen into the descending colon. The colon then curves back into the sigmoid colon then turns into the rectum. Documentation alert: Even if you’re familiar with colon anatomy, you never want to assume to which part of the colon the gastroenterologist referred to. Always ask the provider for clarification if the documentation is unclear. Note also that if the pathology report isn’t back, you may have to use the generic polyp code K63.5 (Polyp of colon), which is not region-specific. Distinguish Between Neoplastic Polyps… While colon polyps are among the most common diagnoses that gastroenterologists see, to code them specifically means to distinguish neoplastic from non-neoplastic polyps. Neoplastic: This type describes abnormal growth with the potential for malignancy being present or to develop if the polyp hadn’t been completely removed. Neoplastic polyps are broken down into more specific classifications as well. Adenomatous polyps (APs) can develop into colorectal cancer, but not all adenomas turn into cancer. Because of the potential for malignancy, most insurers will reimburse follow-up and surveillance procedures for patients who have adenomatous polyps. Patients with APs are usually designated as having a history of colonic polyps, which codes to Z86.010 (Personal history of colonic polyps). Look for these terms: Instead of calling it an adenoma, the pathology report may also categorize the polyp in one of two ways. “A tubular adenoma is the most common type of benign but potentially cancerous polyp,” says Glenn D. Littenberg, MD, MACP, FASGE, AGAF, a gastroenterologist and former CPT® Editorial Panel member in Pasadena, California. “A villous adenoma (or villotubular adenoma) of the colon is a more advanced polyp, closer to malignancy with a different glandular structure, and is sometimes a carpet-like polyp. Unlike coding for adenomas, the only ICD-10 code for villous polyps is D37.4 (Neoplasm of uncertain behavior of colon), a subcategory of D37 (Neoplasm of uncertain behavior of oral cavity and digestive organs) describing neoplasm of an uncertain behavior, with the fourth digit (1 to 4) specifying the exact location.” Combination: Occasionally, a polyp is a reported as a sessile serrated lesion/ adenoma, which microscopically has some features of a hyperplastic polyp but has a behavior (cancer potential) of an adenoma. These should be coded using the D12.- series based on location. It’s also common for patients to have multiple polyps of different morphologies, such as hyperplastic polyps and AP s in different locations. If the polyps have different diagnoses, you can report one for each type of polyp. Adenocarcinomas: When an adenomatous polyp becomes cancerous, it is called an adenocarcinoma and is malignant. Sometimes a neoplastic polyp will contain an area of adenocarcinoma. In these reports, the designation may be “high grade dysplasia” (or older term, “carcinoma in situ”). In this situation, you’d report D01.1 (Carcinoma in situ of rectosigmoid junction) and D01.0 (Carcinoma in situ of colon), depending on the location. … And Non-Neoplastic Polyps These are typically comprised of normal tissue or harmless tissue (for example, a hyperplastic polyp), and fall into the following categories: Don’t Code for Polyps Prematurely Once you have all of the above information locked in, remember the importance of waiting for the pathology report before selecting your polyp codes. To choose the correct ICD-10 diagnosis code for a colon polyp, you will need to know whether the polyp is benign or malignant. You will have to correctly interpret the pathological descriptions used in the report to translate those descriptions into the right category. Gastroenterologists may imply what type of polyp is indicated in an operative report, but they usually defer to the pathology report before making a final recommendation about when the colonoscopy should be repeated, as the path report contains the definitive determination of a colon polyp’s behavior. Tip: The final pathology report will be the determining factor on whether a polyp is non-neoplastic or neoplastic. This differentiation is important in selecting the proper time interval for a follow-up colonoscopy. Although most polyps do not usually turn cancerous, they may cause gastrointestinal problems such as bleeding and obstruction. Heads up: The pathology report is also important because it may also provide information on whether the polyp is primary, secondary, or in situ in case of malignancy. For reporting malignant polyps, you should apply the code that refers to a specific location within the colon from the diagnosis code range C18.- (Malignant neoplasm of colon), with a code for cancer in overlapping regions (C18.8), or with a code for an unspecified location (C18.9). You can also choose from C19 (Malignant neoplasm of rectosigmoid junction) or C20 (Malignant neoplasm of rectum) for rectal region malignancies. Coding alert: If you bill the procedure before the pathologic diagnosis is back from the lab, colon polyps that appear benign are coded with K63.5 (Polyp of colon) in nearly all the circumstances above. If a final pathologic diagnosis is back before billing, then the more specific code is reported.