Master GI Tube Coding In 6 Steps
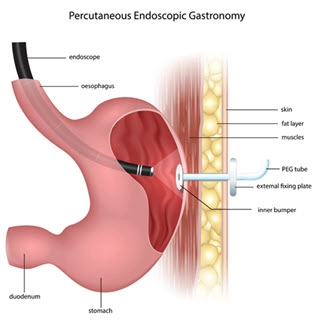
Find the coding secret for gastro-jejunostomy tube insertion When you see an op note that includes placing, repairing, or removing a tube from somewhere in the patient’s gastrointestinal (GI) tract, you don’t have a simple sequential list of codes to deal with. Instead, you’ll find the codes you need scattered throughout the CPT® Surgery/Digestive System chapter with a host of guidance sprinkled in. Let our experts help you find the right code for your case in six easy steps, so your coding efforts don’t go down the tubes. Step 1: Remember the Anatomy You hear “G-tube” and “PEG” thrown around whenever tube coding is on the table. G-tube means “gastric tube” and PEG means “percutaneous endoscopic gastrostomy,” but not every tube goes into the stomach. Know the parts: The GI tract leading out of the mouth and esophagus starts with the stomach and is referred to by the terms “gastric” or “gastro.” The rest of the GI tract is comprised of the following: While you’re considering the terminology to decipher the codes, you should also remember that an “ostomy” refers to a surgery that creates a stoma (opening) from inside the body to outside the body, typically to allow bodily contents or nutrition to pass through a tube. Step 2: Distinguish Tube Placement by Anatomic Site CPT® provides the following codes for surgical procedures to place a tube somewhere in the GI tract: Using your knowledge of the GI tract, you’ll select the appropriate code based on the surgeon’s documentation of where they placed the tube. Step 3: Focus on the ‘Vision’ Once you decipher the correct code based on anatomic site, you can see that you’re left with two choices for a gastric tube placed in the stomach. If the surgeon performs an esophagogastroduodenoscopy (EGD) and places the tube percutaneously while visualizing the site through the scope, you should report 43246. On the other hand, if the surgeon doesn’t perform an EGD but uses fluoroscopic guidance to guide the tube placement from outside the body, you should turn to 49440. All inclusive: In the 49440 procedure, the surgeon punctures the abdominal wall from outside the body and inserts a device under fluoroscopic guidance to pull the stomach up to the abdominal wall for percutaneous tube insertion. Code 49440 includes all components of the service, so you should not separately code the fluoroscopic imaging, according to Marcella Bucknam, CPC, CCS-P, COC, CCS, CPC-P, CPC-I, CCC, COBGC, revenue cycle analyst with Klickitat Valley Health in Goldendale, Washington. Step 4: Use These “Replacement” Codes When the surgeon replaces a tube under fluoroscopic guidance, you shouldn’t use the tube placement codes. Instead, you have an entirely different set of codes to describe the work, as follows: Anatomy: You can see that selecting the proper replacement code depends on the anatomic site of the tube, similar to the placement codes. No guidance: If the surgeon performs percutaneous tube replacement without guidance, you should turn to one of the following two codes depending on the surgeon’s documentation of gastrostomy tract revision: Step 5: Don’t Miss the Tube ‘Maintenance’ Services Sometimes the physician needs to evaluate a tube that’s already in place, or clear a tube that is obstructed. CPT® provides the following two codes for those scenarios: Conversion: When the physician converts a gastrostomy tube to a gastro-jejunostomy tube, report 49446 (Conversion of gastrostomy tube to gastro-jejunostomy tube, percutaneous, under fluoroscopic guidance including contrast injection(s), image documentation and report). Problem: Sometimes the surgeon places a gastro-jejunostomy tube in the initial operative session, but there’s no code for that. The procedure involves a dual-lumen tube, typically for a feeding tube. The surgeon might use the gastric lumen for decompression, while the jejunal lumen administers nutrition. Solution: “You should report placement of a gastro-jejunostomy tube using two codes, even though the surgeon performs the work in one session,” says Terri Brame Joy, MBA, CPC, COC, CGSC, CPC-I, revenue cycle director for Clinical Health Network for Transformation in Houston, Texas. The two codes are 49440 for the gastrostomy and 49446 for the conversion. CPT® affirms this coding with a text note following 49446 that states, “For conversion to a gastro-jejunostomy tube at the time of initial gastrostomy tube placement, use 49446 in conjunction with 49440.” Step 6: Avoid These “Removal” Errors If your surgeon simply removes a tube from the GI tract and doesn’t replace it with anything, you won’t find a procedure code for the work. Some coders have asked if that’s reportable as a tube repair (such as 49460) or foreign body removal (such as 43247, Esophagogastroduodenoscopy, flexible, transoral; with removal of foreign body(s)). The answer is no. Instead, you should report the service using an office and other outpatient evaluation and management (E/M) code (99202-99215) as appropriate based on the surgeon’s documentation. Question: Here’s another common question about G-tube removals: During an EGD procedure, the surgeon removed the flange from a worn out G-tube and then introduced a new feeding tube. Should we report 43247 for the flange removal and 43246 for the new tube placement? Answer: Again, the answer is no. The insertion procedure includes removal of an existing tube. The only code you should report for this situation is 43246.