Medicare Pay Increase Is On The Way, But Labor Share Change Muddies Hospices’ Reimbursement Picture
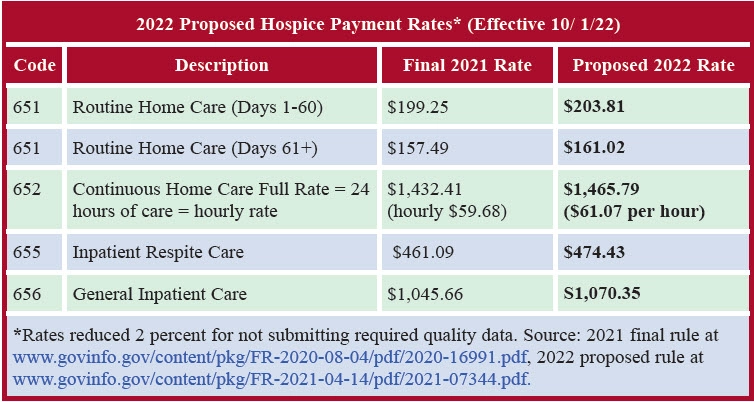
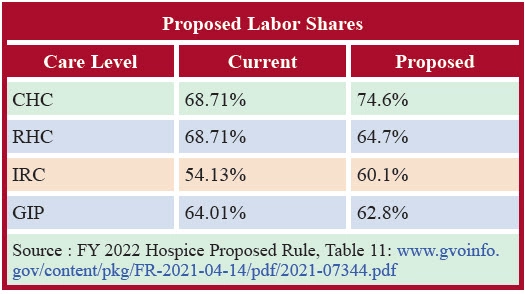
You could end up with lower payment rates than you currently receive, depending on where your agency is located. You’ll see a 2.3 percent increase to your Medicare reimbursement rates next year, if a new proposal is finalized. Under the proposed rule published in the April 14 Federal Register, “hospices would see a 2.3 percent ($530 million) increase in their payments for [fiscal year] 2022,” the Centers for Medicare & Medicaid Services says in a fact sheet about the rule. “The proposed 2.3 percent hospice payment update … is based on the estimated 2.5 percent inpatient hospital market basket reduced by the multifactor productivity adjustment (0.2 percentage point),” CMS explains. As always, “hospices that fail to meet quality reporting requirements receive a 2 percentage point reduction to the annual market basket update for FY 2022,” the agency adds. Also as always, the 2.3 percent rate of increase is not set in stone. “If more recent data becomes available … before the publication of the final rule … we would use such data … to determine the hospice payment update percentage for FY 2022 in the final rule,” CMS notes in the rule. Last year, CMS lowered the update from a proposed 2.6 percent in the proposed rule to a smaller 2.4 percent in the final rule (see HOP, Vol. 13, No. 9). “We support the proposed 2.3 percent rate update,” says the National Hospice and Palliative Care Organization in comments shared with AAPC. “Hospice and palliative care providers face significant hardship as they continue to serve patients and their families during the COVID-19 pandemic. CMS should recognize this as they fulfill their commitment to support providers both through regulation and the subregulatory process,” the trade group says. Cap: “The proposed hospice cap amount for the FY 2022 cap year will be $31,389.66, which is equal to the FY 2021 cap amount ($30,683.93) updated by the proposed FY 2022 hospice payment update percentage of 2.3 percent,” the rule says. Like the rate update, the cap increase may also be subject to change, points out the National Association for Home Care & Hospice in its member newsletter. Unlike the payment rates, the per-beneficiary cap “is not currently wage adjusted,” highlights consulting firm The Health Group in Morgantown, West Virginia. High Wage Index Hospices Beware Another proposal may have a significant impact on your individual agency’s bottom line next year, however. CMS says it wants to “rebase and revise the labor shares for continuous home care (CHC), routine home care (RHC), inpatient respite care (IRC), and general inpatient care (GIP) using 2018 Medicare cost report (MCR) data for freestanding hospice facilities,” according to the rule. Old way: In 1984, CMS based the labor share for CHC and RHC on home health data, the rule says. CMS based the IRC and GIP labor share amounts on skilled nursing facility data. New way: CMS proposes using five data elements from cost reports to set the new labor share — (1) Direct patient care salaries and contract labor costs, (2) direct patient care benefits costs, (3) other patient care salaries, (4) overhead salaries, and (5) overhead benefits costs. CMS will use a sample of cost reports and will derive data for inpatient levels only from cost reports of agencies that provided that level of care, the rule says. CMS offers information to head off criticism of its sampling process. “We conducted sensitivity analysis to test for the representative of this sample by reweighting compensation cost weights using data from the universe of freestanding providers that reported either IRC or GIP total costs,” the rule details. “For example, we calculated reweighted compensation cost weights by ownership-type (proprietary, government and nonprofit), by size (based on RHC days) and by region.” The result seems to satisfy CMS. “Our reweighted compensation cost weights for IRC and GIP were similar (less than one percentage point in absolute terms) to our proposed compensation cost weights for IRC and GIP,” the agency says in the rule. “Therefore, we believe our sample is representative of freestanding hospices providing inpatient hospice care.” NAHC plans “to closely examine the revisions to the labor share of the payments to assess CMS’ approach and their impact,” the association’s Theresa Forster tells AAPC. “Of specific interest is the fact that the labor share for routine home care is dropping by approximately 6 percentage points. That could have a significant impact for providers with wage index values over 1.0, particularly given that RHC is such a large portion of every hospice provider’s care days,” Forster points out. You shouldn’t assume your rates are increasing based on the topline 2.3 percent bump. “On an individual basis the labor share changes could have some impact,” advises M. Aaron Little with BKD in Springfield, Missouri. “For those hospices serving an area that is proposed to see an increase in the wage index adjustment, those hospices won’t get as much benefit due to the proposed decrease in the routine home care labor share,” Little explains. On the other hand, “those hospices serving an area that is proposed to see a decrease in the wage index adjustment should see less of an impact due to the proposed labor share change.” An example: Little offers a case study from one of his clients. “Despite the estimated overall national net increase of 2.3 percent, after considering the wage index adjustments in their service area and the change in the labor share, they are projected to see a benefit of only 1 percent,” he illustrates. “They’re still grateful for the small increase, but [it’s] a good example of how these proposed changes can impact individual providers.” Hospices will have a chance to share their feedback on the proposal with CMS. Comments are due June 7, CMS notes in its fact sheet. In particular, “we invite comments on our proposed methodology to derive the labor shares for each level of care,” the rule says. “I encourage you to review the proposed rule with your team and provide comment to CMS by the deadline,” says Mary Madison, clinical consultant with Briggs Healthcare on the company’s blog. “Make your voices heard,” Madison urges. Note: The 75-page rule is at www.govinfo.gov/content/pkg/FR-2021-04-14/pdf/2021-07344.pdf. A link to the proposed wage index changes is at www.cms.gov/medicaremedicare-fee-service-paymenthospicehospice-regulations-and-notices/cms-1754-p.