Hospices' 2017 Pay Increase Improves Over Proposal -- But Only A Bit
Hospices are slated to receive an additional $350 million in Medicare payments next year.
In the final rule released July 29, the Centers for Medicare & Medicaid Services adopts the policies largely as proposed back in April (see Eli’s Hospice Insider, Vol. 9, No. 6). The final rule contains “no big surprises,” observes Theresa Forster with the National Association for Home Care & Hospice.
One welcome change, however, is a slight uptick in the payment increase that will begin Oct. 1.
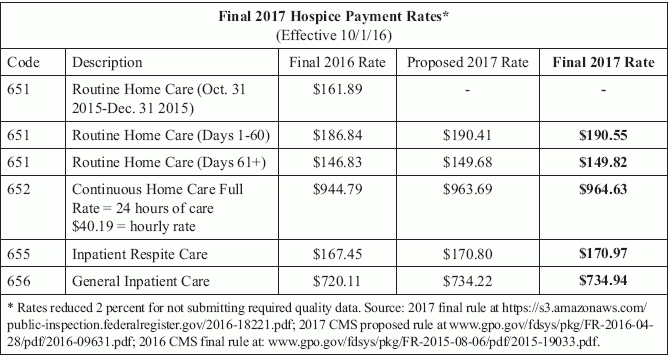
Breakdown: CMS will increase hospice payment rates by 2.1 percent in fiscal year 2017, a slight increase from the proposed 2.0 percent. The update reflects an estimated 2.7 percent inpatient inflation update, reduced by a 0.3 percent productivity adjustment and a 0.3 percent adjustment required by the Affordable Care Act, CMS notes in a release about the rule. (See specific service rates in chart, p. 66.)
Productivity factor reduced: CMS originally estimated a 2.8 percent inflation update reduced by a 0.5 percent productivity adjustment.
Thanks to the slightly increased update factor, the cap amount for 2017 will also be slightly higher than proposed — $28,404.99 instead of the $28,377.17 CMS originally floated.
CMS also forges ahead with its plan to change the cap year timing. “The 2017 cap year will start on October 1, 2016 and end on September 30, 2017,” according to the rule published in the Aug. 5 Federal Register. The change aligns the cap accounting year with the federal fiscal year, CMS notes in its release.
Watch out: The change “will have an impact on when hospices must submit their self-calculated Aggregate Cap starting with the 2017 Cap Report,” NAHC warns in its member newsletter. Hospices must “complete their aggregate cap determination not sooner than 3 months after the end of the cap year, and not later than 5 months after, and remit any overpayments,” CMS reminds providers in the rule. “Those hospices that fail to timely submit their aggregate cap determinations will have their payments suspended until the determination is completed and received by the Medicare Administrative Contractor.”
Resource: Check out Table 26 in the rule, which outlines how to count beneficiaries for the cap during the transition time frame.
No Exceptions To New CBSAs
Another reimbursement-related change is the full adoption of Office of Management and Budget Core Based Statistical Area delineations. One agency protested its CBSA make-up, but CMS shot down the complaint. “We believe that the OMB’s CBSA designations reflect the most recent available geographic classifications and are a reasonable and appropriate method of defining geographic areas for the purposes of wage adjusting the hospice payment rates,” CMS says in the final rule. “We do not see any compelling reason to deviate from the OMB designations.”
This year’s rule contained relatively few reimbursement changes, compared to last year’s rule with sweeping hospice payment reform including the splitting of the Routine Home Care payment rate and addition of Service Intensity Add-on payments. This year’s rule was more focused on quality items (see related stories, this issue).
Note: The final rule is at https://www.gpo.gov/fdsys/pkg/FR-2016-08-05/pdf/2016-18221.pdf.