Random-Order Diagnoses Could Cost You

Implement this ICD-10 action plan to decide which diagnosis should go first.
In situations when your patient presents with more than one diagnosis, relying on your EHR or computer software to rank the diagnoses could mean your claims don’t represent medical necessity. To fix the problem and continue collecting your reimbursement, code based on these ICD-10 guidelines.
A Codify Subscriber wrote to Pediatric Coding Alert asking, “Should I enter the diagnosis codes in the order the provider lists them, or should I start with the presenting diagnosis?” Read on to determine exactly which diagnoses should go first.
List the Most Important Reason First
You should first code the main or most serious diagnosis, which is typically determined as follows:
After the primary diagnosis, you’ll then list additional diagnoses describing other conditions that the patient has as well. “Code all documented conditions that coexist at the time of the encounter/visit, and require or affect patient care treatment or management,” the ICD-10 manual states. “Do not code conditions that were previously treated and no longer exist. However, history codes (Z80-Z87) may be used as secondary codes if the historical condition or family history has an impact on current care or influences treatment.”
Choose Definitive Over Presenting
Be careful that you don’t assume the primary reason for the encounter is the same as the presenting diagnosis. Do this: Instead of focusing on the presenting problem or chief complaint, look for the pediatrician’s definitive diagnosis.
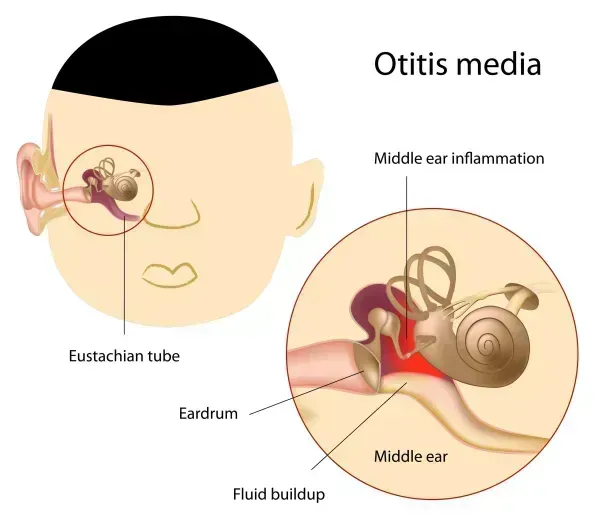
For example: A child comes in because of fever and right ear pain, and the pediatrician finds acute suppurative otitis media. You should first code the definitive diagnosis (H66.001, Acute suppurative otitis media without spontaneous rupture of ear drum, right ear), not the presenting diagnoses (R50.9, Fever, unspecified; and H92.01, Otalgia, right ear). Because the ear pain and fever are “inherent” in the diagnosed condition, you should not separately report them.
Code Symptoms in These Instances
Some circumstances, however, do warrant assigning additional ICD-10 codes for a patient’s symptoms:
1. If the child’s symptoms are not part of the disease process, you should separately code them. A classic example of this involves a child who presents with pneumonia and vomiting. In this case, coding the symptom of vomiting in addition to the pneumonia shows that the child is sicker than if he just had pneumonia. Listing both ICD-10 codes (such as J18.9, Pneumonia, unspecified organism and R11.10, Vomiting, unspecified) would potentially support a higher level of E/M code.
2. When a pediatrician does not establish or confirm a diagnosis, you may report the patient’s symptoms. Suppose a pediatrician sees a child who has just hurt his left elbow, and the physician finds no fracture. Following ICD-10 guidelines, you would use the signs and symptoms and code for the injury (S59.902A, Unspecified injury of left elbow, initial encounter).
Double-Check Your Submission
If you’re in doubt over which ICD-10 code to list first -- or at all -- on a claim form, check whether the diagnosis supports medical necessity for the service or procedure and that it is clearly documented as the physician’s final diagnoses in the medical record. Plus, you should ensure that you’ve assigned the most specific ICD-10 code possible. In some cases, you may find that your diagnosis is too broad and will lead to recoupments down the line.
In addition, if your EHR is automatically determining the first-listed diagnosis code, ensure that your staff members are checking the primary diagnosis before the claim goes out the door.