Locate, Use Common GI Codes Easily With This Tool
And refine your coding accuracy with some expert advice. Patients reporting with gastrointestinal (GI) conditions maybe a common occurrence in your practice, but when you have to choose between two different codes for diarrhea and 45 different hernia codes, finding the precise ICD-10 codes can be quite a challenge. So, we've put together this handy quick-reference guide to 25 of the most common GI diagnosis codes for you to clip and save for future reference. And we've also asked a couple of master coders for their insights and recommendations for fast, accurate documentation. Expert Tip 1: Know When to Code Sign, Symptom, or Definitive Rx Kent Moore, senior strategist for physician payment at the American Academy of Family Physicians, reminds coders that "whether you gravitate to the R or K sections depends on whether you're coding signs and symptoms (R) or a definitive diagnosis (K)." This will help you make the correct choice between two codes that appear to be the same. For example, Moore explains that "R19.7 [Diarrhea, unspecified] represents a sign or symptom of some other underlying condition, which the physician may or may not have diagnosed yet. In comparison," Moore goes on, "K59.1 [Functional diarrhea] represents a definitive diagnosis of a functional intestinal disorder. Basically, the person has diarrhea because his or her bowels don't function properly, not because of some other underlying cause like food poisoning or a virus, for example." The same is true for heartburn. Chelle Johnson, CPMA, CPC, CPCO, CPPM, CEMC, AAPC Fellow, billing/credentialing/auditing/coding coordinator at County of Stanislaus Health Services Agency in Modesto, California, suggests that you code R12 (Heartburn) "if the condition is not considered to be chronic and does not show the various symptoms of GERD." While K21.- (Gastro-esophageal reflux disease) is another form of acid reflux, Johnson notes that "GERD can have additional symptoms, such as heartburn, chronic cough, difficulty swallowing, and in some cases laryngitis." Expert Tip 2: Root Cause Key to Dyspepsia Coding K30 (Functional dyspepsia), also known as indigestion, presents another problem for coders, as it can easily be confused with F45.8 (Other somatoform disorders), which is a catch-all code that includes psychogenic dysphagia among its conditions. Johnson reminds coders that the two share similar symptoms, such as stomach pain, bloating, heartburn, nausea, vomiting, and burping, but K30 "may be caused by an ulcer or acid reflux disease, in which case the underlying cause should be coded first. Nervous dyspepsia's root cause is different," Johnson goes on. "It's an anxiety disorder not caused by a disorder in the esophagus," she explains. Expert Tip 3: Learn These 4 Codes, Rules for Simple Hernia Reporting The American Academy of Family Physicians (AAFP) provides a very useful tip for coders trying to find a precise hernia code among those listed in ICD-10. "Most primary care physicians," the AAFP notes, "will use only four of the 45 hernia codes": But if you have to search further, the AAFP advises that you don't look to code laterality when coding hernias. While many ICD-10 codes specify whether the condition exists on the patient's left or right side, hernia codes are classified by location - they are either inguinal (K40), femoral (K41), umbilical (K42), ventral (K43), diaphragmatic (K44), other (K45), or unspecified (K46). Even those that may occur unilaterally (e.g. inguinal or femoral) don't require you to know which side is involved when it's unilateral. Expert Tip 4. "Consistent With" Doesn't Mean Definitive Even when your provider sends out for labs, and the report comes back, you should not immediately leap to a K code conclusion. The AAFP also notes that "when the test results use a term like 'consistent with,' this is not considered a definitive diagnosis. Unfortunately," the AAFP point out, "this term appears on many pathology reports."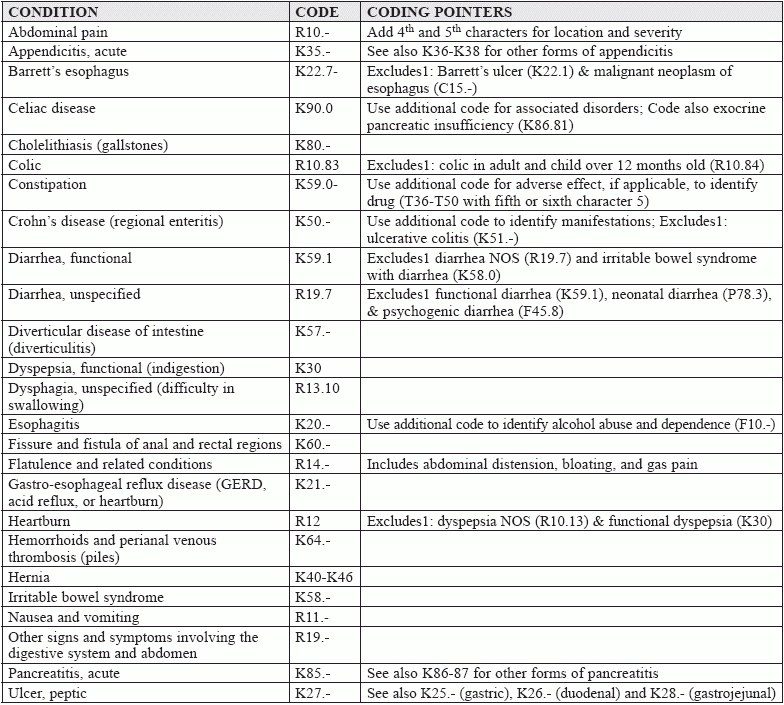
(List adapted from the American College of Gastroenterology http://patients.gi.org/topics/common-gi-symptoms/ and the American
Academy of Family Physicians https://www.aafp.org/fpm/2015/0100/p19.html)


-min.webp)
