Ask These Questions, Get Ready for Behavioral Health Integration

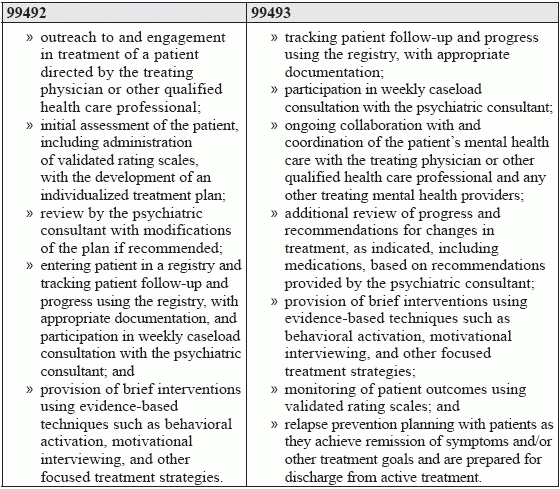
Read this FAQ to know the pros and cons of the new CPT® codes If your practice has yet to embrace behavioral health integration (BHI) or the related new psychiatric collaborative care model (CoCM) of BHI, chances are that it could sometime in the future. That's because, as we discussed in the previous issue of Internal Medcine Coding Alert, CPT® has introduced four new codes specifically related to these models of primary care. These four codes, which take effect on Jan. 1, have raised a number of questions among coders. So, we asked our experts for their answers and compiled them in this handy FAQ in order to keep your coding knowledge up to date. What are CoCM and BHI? The Centers for Medicare and Medicaid Services (CMS) describes CoCM as "a model of behavioral health integration that enhances 'usual' primary care by adding two key services: care management support for patients receiving behavioral health treatment; and regular psychiatric interspecialty consultation to the primary care team, particularly regarding patients whose conditions are not improving" (Source: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/PhysicianFeeSched/Downloads/Behavioral-Health-Integration-Fact-Sheet.pdf). BHI is similar to CoCM in that it includes "'core' service elements such as systematic assessment and monitoring, care plan revision for patients whose condition is not improving adequately, and a continuous relationship with a designated care team member," according to CMS. What conditions are eligible? CMS defines eligible conditions as "any mental, behavioral health, or psychiatric condition being treated by the billing practitioner, including substance use disorders, that, in the clinical judgment of the billing practitioner, warrants BHI services." CMS also says that "beneficiaries may, but are not required to have, comorbid, chronic, or other medical condition(s) that are being managed by the billing practitioner." What are the new CPT® codes for CoCM? Beginning Jan. 1, you will have three CoCM codes to choose from: You would use 99492 (initial) to document the first 70 minutes in the first calendar month and 99493 (subsequent) to document the first 60 minutes in a subsequent month. 99494 (initial or subsequent) is the add-on code to document an additional 30 minutes' service during a calendar month. What clinical responsibilities do the codes require? Per the codes' descriptors, each service has a number of very specific components: How does the new BHI code differ? Kent Moore, senior strategist for physician payment at the American Academy of Family Physicians, identifies four key differences between the new BHI code, 99484 (Care management services for behavioral health conditions, at least 20 minutes of clinical staff time, directed by a physician or other qualified health care professional, per calendar month ...) and 99492-99494. "First," Moore says, "it does not require a psychiatric consultant to be part of the model"; second, clinical staff who "do not have the same level of formal education or specialized training in behavioral health associated with behavioral health care managers" can administer it; third, "the time threshold is lower, and the time associated with the code is open-ended; i.e., there is no time-based add-on code available with 99484"; and, fourth, the clinical responsibilities differ. For 99484, those responsibilities include Will tracking the clinical responsibilities of the new codes be difficult? "The problem," as Suzan Hauptman, MPM, CPC, CEMC, CEDC, AAPC Fellow, senior principal of ACE Med in Pittsburgh, sees it, "is who documents? Where is the documentation? Keep in mind each clinician must write his or her own note. Clinicians don't always document in the same place around the same time for a service that is collaborative." To deal with this, Moore suggests practices should, or need to, set up "systems to ensure the required elements of the code(s) are met each month for which the code(s) are billed and to track the necessary time." Moore encourages coders to be involved in planning those systems, "so they have confidence that all elements have been met when reporting code(s) for a given month." It's a suggestion wholeheartedly supported by Hauptman, who believes that "coders will need to work with the clinicians to come up with a template or process for documenting these services so that they can be reported compliantly."