PQRS Reporting: Ethical Coding By Selecting Right Options

Hint: Base your decisions by analyzing the number of providers in your group.
If you’re contemplating whether or not to have your family practice participate in the Physician Quality Reporting System (PQRS), you’ll need to decide whether to join as a group or to enter your practitioners as separate individuals.
Decide on Individual vs. Group Reporting
Eligible providers have an option to report as either an individual or a group to earn their PQRS incentive.
As an individual, your PQRS quality measures are reported using your national provider number (NPI). However, the incentive payment is provided to the tax identification number (TIN) of the reporting entity. An individual may report using traditional claims and the appropriate quality data codes on the claim form as part of the billing process. You may also report through a qualified registry in 2013, if you have access to one.
Third option: Of note, there is a third option of reporting via an electronic health record (EHR), if your EHR supports that option.
Group practices with 99 or fewer eligible professionals must decide if they want to continue to report as individuals using one of the multiple reporting options for individuals described above, or if they would like to participate as a group. Group participation is referred to as the Group Practice Reporting Option (GPRO.
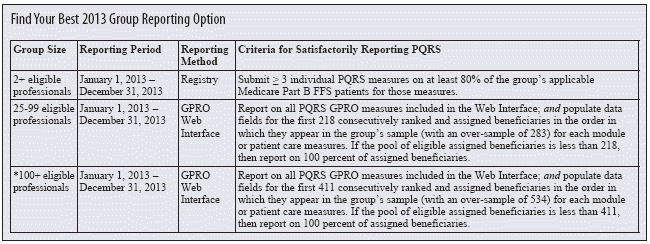
2013 change: For the 2013 PQRS, CMS changed the definition of a group practice under the GPRO to start at two or more eligible professionals practicing under the same TIN. “In 2010, the GPRO was only for groups with over 200 Eligible Professionals (Providers),” explains Jill M. Young, CPC, CEDC, CIMC, principle of Young Medical Consulting LLC in East Lansing, Mich. “In 2013, they have made a sort of small, medium and large distinction in the GPRO. Just remember, the reporting requirements are different for each of the three sizes.”
Group practices of 100 or more eligible professionals will be subject to a separate Value-Based Modifier (VBM) in 2015 based on their 2013 performance under PQRS. Such groups must self-nominate to report quality data as a GPRO and would typically elect to be reviewed using the administrative claims options described below. Unlike the individual reporting options, those who want to participate as a group must elect to do so by submitting a self-nomination statement via the web from July - Oct. 15, 2013. In the meantime, your group practice can set up your Individuals Authorized to Access CMS Computer Services (IACS) account. Only this authorized user can elect your GPRO, warns Beck.
Review the Group Reporting Options
If you’re reporting your quality data using the group designation, you should get familiar with three reporting options you might use. “There are different options, and you have to look at what is most appropriate for you,” Young explains. (See more details about each group level in the chart from Young).
GPRO Web Interface: The GPRO Web Interface is only available to group practices of 25 or more eligible professionals. Groups electing this option will report on a set of 18 primary care and prevention measures.
Note that this option is not recommended for emergency department only or hospital-based TINs and will not meet the criteria for the incentive for hospital-based group practices, Beck says.
GPRO Qualified Registry: CMS will offer group practices consisting of two or more eligible professionals the option to report PQRS measures through qualified registries. This is a new reporting option for group practices and actually the only option that smaller group practices (2-24 professionals) can use to qualify as a group for the 2013 PQRS incentive.
GPRO Administrative Claims Option: The new administrative claims option provides groups with an additional opportunity to avoid the 2015 PQRS and VBM penalties. Under this option, CMS will analyze a group’s Medicare claims for a set of 17 measures for assigned beneficiaries, and specific quality data codes do not have to be submitted to CMS. CMS has agreed that for groups who elect this option, even if they have a denominator of zero for all measures, they can still avoid the 2015 PQRS penalty for this option only.
Participation in the new administrative claims option does not earn a PQRS incentive. However, if a group practice elects to use the administrative claims option, the individual eligible professionals may still use the traditional claims or registry reporting mechanisms to qualify for the 2013 PQRS incentive, Beck explains.
Bottom line: You need to figure out where your practice falls in the guidelines, based on the number of providers you have reporting together as a group, and then get to know the details and requirements associated with reporting at that level, Young says.
For more information on PQRS, visit the CMS link at http://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/PQRS/index.html.