Don't Miss These Section A Changes Come October
Ensure you know which of these options have been removed or modified.
Gear up for the myriad changes to the MDS 3.0 that the Centers for Medicare & Medicaid Services (CMS) has incorporated in its most recent draft Nursing Home Comprehensive (NC) item set for version 1.14.0 effective Oct. 1, 2014.
Heads Up: 4 Section A Changes Coming
Many of the more significant changes will occur in Section A — Identification Information. In this section, CMS plans to:
1. Remove response option 06 — Readmission/return from A0310B — PPS Assessment. CMS is eliminating this option because it is the functional equivalent of the 01 — 5-day scheduled assessment response option.
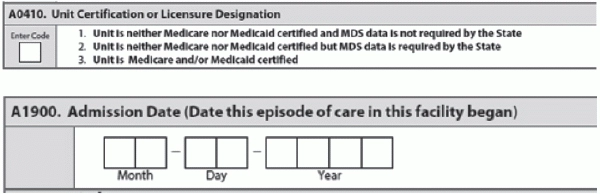
2. Change the verbiage in item A0410 — Submission Requirement. The language changes won’t become effective until after the Sept. 12 CMS downtime. Item A0410 will now be titled Unit Certification or Licensure Designation, and will include the following reworded response options:
3. Remove A1500, A1510 and A1550 Preadmission Screening and Resident Review (PASRR) items from all item sets except for the NC. PASRR items are active on some sets prior to Oct. 1, 2014, but they will no longer be collected on the NP (PPS) or NQ (QR).
4. Add A1900 — Admission Date (Date this episode of care in this facility began), which is tied to items A1600 — Date of Admission or Reentry, A1700 — Type of Entry, and A1800 — Entered From. A1900 will correlate/work with the Quality Measures and will tie all records in a stay together, as well as tie all records in an episode together, CMS notes.
“A1900 will remain the same as the original admission date in the face of a discharge return anticipated and the resident returns within 30 days,” CMS states. “A1600 will reflect the return/reentry date, but the A1900 will be the original admission date.”
Coding for A1900 would change when the resident has a discharge return not anticipated or discharge return anticipated and the resident fails to return to the facility within 30 days. In that case, A1900 is the new date of admission when the resident returns.