Complete This MDS Paperwork When a Resident Dies
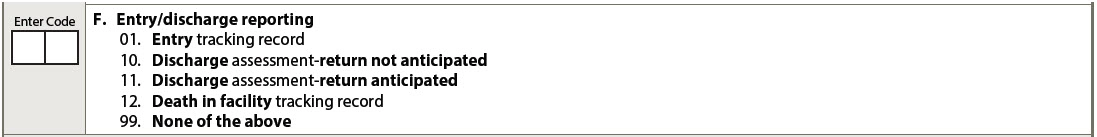
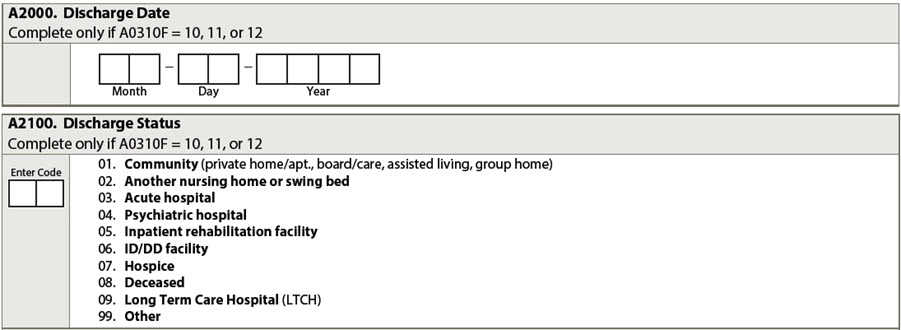
Hint: A Part A Discharge Assessment probably isn’t necessary. Every person who works in a nursing home or skilled nursing facility is familiar with death — and now, more than ever, 17 months into a pandemic that has hit the elderly the hardest. The Centers for Medicare & Medicaid Services (CMS) classifies death as one type of discharge from a facility, which means that there is paperwork you need to complete when a resident dies. Read on for more information on the particulars of what to do in the event of a resident death, from paperwork and compliance to tips to managing resident and staff grief. Understand Coding Responsibilities A resident’s death must be coded on the MDS; CMS considers a death in the facility a type of discharge. You need to complete the death in facility tracking record, as well as code the specifics of the “discharge.” All of these items are in Section A (Identification Information) of the MDS. One implicated item (A0310F Entry/discharge reporting) includes the Death in facility tracking record, which involves some special submission/transmission responsibilities. “For Entry and Death in Facility tracking records, the MDS Completion Date (Z0500B) must be no later than 7 days from the Event Date (A1600 for an entry record; A2000 for a Death in Facility tracking record),” the RAI Manual says. This information must be transmitted within 14 days. For A2000 (Discharge Date) and A2100 (Discharge Status), you’ll need to code the date of death on the discharge date and then code the discharge status as 08. Deceased. Note that the Death in Facility Tracking Record must be completed for any resident dying in the facility or while on a leave of absence. If you make an error when filling out the Death in Facility Tracking Record (A0310F), the provider must take the following actions to correct the record. the RAI Manual says on page 5-11: Skip This Assessment in This Situation If the resident’s days of Medicare-covered care run out on the same day that the resident dies, you need only complete a Death in Facility Tracking record. “If the End Date of Most Recent Medicare Stay (A2400C) occurs on the same day that the resident dies, a Death in Facility Tracking Record is completed, with the Discharge Date (A2000) equal to the date the resident died. In this case, a Part A PPS Discharge assessment is not required,” the RAI Manual says. If you’re in the midst of assessing a resident when they die, you do not need to finish the assessment. “If a resident dies prior to the completion deadline for the assessment, completion of the assessment is not required. Whatever portions of the RAI that have been completed must be maintained in the resident’s medical record. In closing the record, the nursing home should note why the RAI was not completed,” the RAI Manual says, on page 2-32. However, timing matters in other situations too. For example, the RAI Manual says that if the Medicare beneficiary dies in the SNF or while on a leave of absence before or on the eighth day of a covered SNF stay, you’ll still need to prepare a 5-day assessment: “… the provider should prepare a 5-Day assessment as completely as possible and submit the assessment as required. If there is not a PPS assessment in the QIES ASAP system, the provider must bill the default rate for any Medicare days.” Beware: If a resident dies or is discharged during the lookback period for a required assessment, you need to adjust the assessment reference date (ARD) to equal the discharge date. “If the resident is skilled, you would want to try to at least get the primary diagnosis established and absolutely any other items that could be completed on the 5-Day so that the facility can get paid for more than the default rate. And then still do a Death in Facility Tracking record,” says Jane Belt, MS, RN, QCP, RAC-MT, RAC-MTA, curriculum development specialist at American Association of Post-Acute Care Nursing (AAPACN) in Denver. “If the beneficiary dies in the SNF or while on a leave of absence before or on the eighth day of the covered SNF stay, the provider should prepare a 5-Day assessment as completely as possible and submit the assessment as required. If there is not a PPS assessment in the QIES ASAP system, the provider must bill the default rate for any Medicare days. The provider must also complete a Death in Facility Tracking Record (see Section 2.6 for greater detail),” the RAI Manual says on page 2-50. “The day of discharge or death is reimbursed when the resident dies or is discharged home or to a non-Medicare-participating provider on the day of admission or readmission,” she says.