Follow 5 Steps To Perfect Your CAA Process & Care Planning
Understand exactly what your CAA Summary should include.
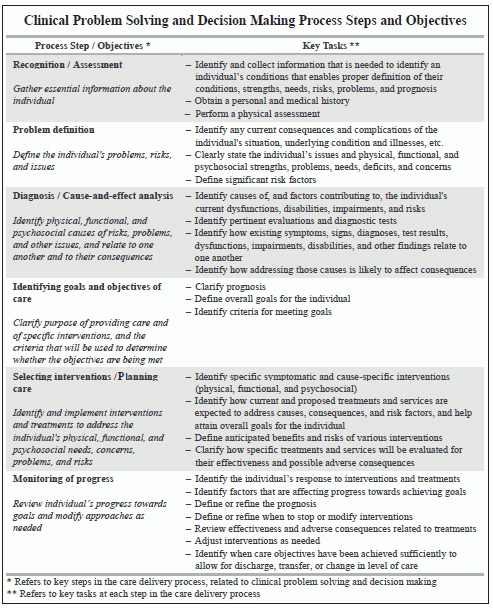
Many MDS Coordinators don’t pay nearly enough attention to Chapter 4 of the RAI manual. But this is where the Centers for Medicare & Medicaid Services (CMS) sets forth its standards for care planning. Here’s what you can learn from MDS experts and Chapter 4 to help improve your Care Area Assessment (CAA) process.
“Chapter 4 of the RAI manual is one of the least read and most important for quality outcomes,” stated consultant Judy Wilhide Brandt, RN, BA, RAC-MT, C-NE, in a March 3 analysis for Washington, D.C.-based Leading Age. Chapter 4 “contains excellent training and examples of how to conduct a thorough assessment to come to the correct care plan problem.”
Step 1: Spot Triggered Care Areas
The CAA process begins, of course, with the MDS assessment. First, you need to identify which care area is triggered and why, according to a recent MDS advanced training by Mary Woodyard, BSN, RN, of the Ohio Department of Health.
“Determine if the care area is a problem for this resident,” Woodyard said. “Describe the nature of the problem and the impact on functioning.”
For instance, coding J1800 — Any Falls Since Admission/Entry or Reentry or Prior Assessment (OBRA or Scheduled PPS), whichever is more recent as 1 — Yes triggers the Falls CAA, Brandt noted. “It is impossible to know how to care plan this area without conducting an investigation.”
Step 2: Review the MDS & Gathered Data
You will have very different interventions if the resident slipped on a puddle of water or if her legs gave way because she had an exacerbation of Parkinson’s disease, Brandt pointed out. And you should also find out when the resident had her last meal, what medications she recently received, any co-morbidity, and how she was feeling emotionally that day.
You should identify “causative and unique risk factors,” including the resident’s potential for improvement or decline and strengths to build on, Woodyard noted.
Bottom line: “When a CAA triggers, it is an invitation to do an exhaustive investigation aimed at improving function when possible, maintaining function when improvement is not possible, or supporting as the elder wishes if decline is imminent,” Brandt said.
When you review the CAA, first consider what MDS items triggered the CAA, and then look for any issues or conditions that may contribute to the CAA but are not necessarily captured in the MDS data.
Step 3: Spark IDT Decision-Making & Care Planning
The next step is for the interdisciplinary team (IDT), along with the resident and/or the resident’s representative, to identify areas of concern, decide if a care plan intervention is necessary, and, if so, determine what types of interventions may be appropriate, Brandt stated.
Also, you need to identify a need for referral. According to Woodyard, the IDT should:
Step 4: Complete Your Documentation
“Document which research, resource(s) or assessment tool(s) were used in completing the CAA, as specified in Chapter 4” of the RAI manual, Woodyard instructed. “What plan of care can be developed/revised to improve status, maintain function and prevent decline?” And if the IDT decides not to proceed with care planning, you must document why.
“While the CAAs can help the IDT identify conditions or findings that could potentially be a problem or risk for the resident, additional thought is needed to define these issues and determine whether, and to what extent, the care area issue and/or condition is a problem or issue needing an intervention,” Brandt cautioned. “Or simply a minor or inconsequential finding that does not need additional care planning.”
Step 5: Write Your CAA Summary
After you’ve gathered all the information, you need to make a clear issue or problem statement, Brandt instructed. And keep in mind that “an issue or problem is different from a finding (e.g., a single piece of information from the MDS or a test result.” An issue or problem is also not the same as the “chief complaint.”
To write good CAAs, you must “paint a picture of the resident’s status,” Woodyard said. “Talk about the resident’s individual condition — the care plan must be individualized.” Use the MDS information and the CAA process to provide the foundation for formulating the individualized care plan.
Important: According to Woodyard, your CAA Summary should:
Bottom line: The CAA process is crucial to effective and meaningful care planning. After all, “if the problem is not correct, the interventions are destined to fail,” Brandt warned.