Make the Right Coding Choices for Therapeutic Diets
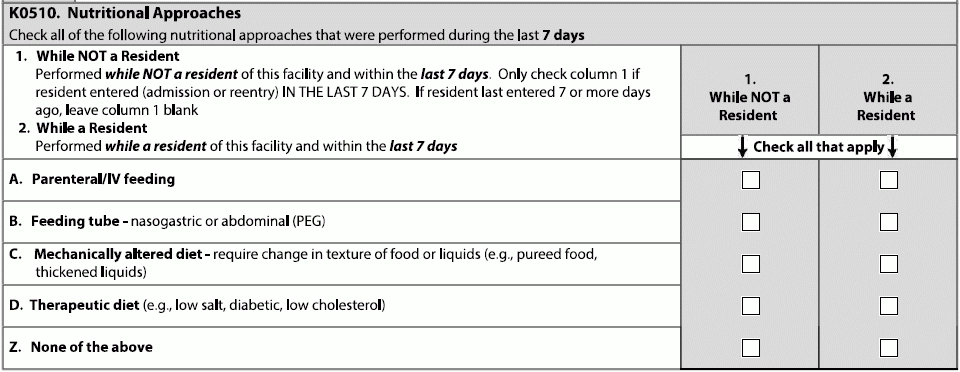
Don’t let misconceptions about fad diets color coding on disease processes. Many people are adopting diets that are meat-free, dairy-free, or gluten-free, but some people may be making those choices because of an underlying health condition. If a resident arrives at your facility with a documented allergy to meat or dairy or gluten and requires a special diet, make sure you’re making the correct coding choices on the MDS. You’ll be setting up the resident for care and meals that are comfortable and safe. Know What Qualifies as ‘Therapeutic’ Celebrities and lifestyle social media influencers may make claims about the “therapeutic” qualities of the diets they espouse, but the clinical definition of therapeutic is a bit stricter. The Resident Assessment Instrument (RAI) Manual defines it as such, on page K-11: “A therapeutic diet is a diet intervention ordered by a health care practitioner as part of the treatment for a disease or clinical condition manifesting an altered nutritional status, to eliminate, decrease, or increase certain substances in the diet (e.g., sodium, potassium) (ADA, 2011).” Documented food allergies that require a specialized diet should be coded as therapeutic on MDS item K0520D (Nutritional Approaches), per the RAI Manual’s definition. So, if you see notes about lactose intolerance or an allergy to animal proteins or gluten sensitivity, you need to note the respective allergy or sensitivity on the MDS, as well as alerting nursing and dietary services and addressing the concerns in the Care Area Assessment (CAA) summaries for Nutritional Status and/or Dehydration/Fluid Maintenance AND including the issue in care plans, says Jane Belt, MS, RN, RAC-MT, RAC-MTA, QCP, curriculum development specialist at American Association of Post-Acute Care Nursing (AAPACN) in Denver. Note: In October 2020, this will become item K0510 (Nutritional Approaches) according to the current MDS draft. Know How to Code Active Diagnoses Food intolerance issues can cause a lot of pain and discomfort for residents. Though working with nutrition services is a major component of caring for a resident with a food intolerance, some issues that can be severe, like celiac disease, do qualify as “Medical Management” under the Patient-Driven Payment Model (PDPM). However, a resident’s general food allergy “status” does not usually qualify as a primary diagnosis, though it is certainly necessary information for their care. Another way to think about food allergies or sensitivities: If the resident had a reaction and is admitted to a facility for follow-up care, the diagnosis for some reactions may qualify as “Medical Management.” Keep These ICD-10 Codes Handy Clip and save the following code chart to keep on hand for residents who have diagnoses surrounding food intolerance or food sensitivity. Note that some, including the T78 codes, require a 7th character; for nursing facilities, that would usually be D = subsequent encounter, i.e., T78.07D (Anaphylactic reaction due to milk and dairy products). » E73.- (Lactose intolerance) » K90.0 (Celiac disease) o K90.41 (Non-celiac gluten sensitivity) » T78.0 (Anaphylactic reaction due to food) o T78.06 (Anaphylactic reaction due to food additives) » Z91.01 o Z91.012 (Allergy to eggs) » Z91.02 (Food additives allergy status) Celebrate Reduction of Antipsychotic Use The Centers for Medicare & Medicaid Services (CMS) notes that the use of antipsychotic medication in nursing facilities is dropping. “We’re excited to share that, for the first time since 2011, there is ~40% [drop] in the prevalence of antipsychotic drug use in nursing homes,” says CMS Administrator Seema Verma, on Twitter. CMS has entered a national partnership with “federal and state agencies, nursing homes, other providers, advocacy groups, and caregivers to improve comprehensive dementia care,” CMS says on its website. “While the initial focus was on reducing the use of antipsychotic medications, the Partnership’s larger mission is to enhance the use of non-pharmacologic approaches and person-centered dementia care practices.” For more information, including the antipsychotic medication use data report from January 2020, look here: www.cms.gov/Medicare/Provider-Enrollment-and-Certification/SurveyCertificationGenInfo/National-Partnership-to-Improve-Dementia-Care-in-Nursing-Homes.
o E73.0 (Congenital lactase deficiency)
o E73.1 (Secondary lactase deficiency)
o E73.8 (Other lactose intolerance)
o E73.9 (Lactose intolerance, unspecified)
» K90.4 (Other malabsorption due to intolerance)
o Exlcudes2 gluten-sensitive enteropathy (K90.0)
• Lactose intolerance (E73.-)
o K90.49 (Malabsorption due to intolerance, not elsewhere classified)
• Malabsorption due to intolerance to carbohydrate
• Malabsorption due to intolerance to fat
• Malabsorption due to intolerance to protein
• Malabsorption due to intolerance to starch
o T78.00 (Anaphylactic reaction due to unspecified food)
o T78.01 (Anaphylactic reaction due to peanuts)
o T78.02 (Anaphylactic reaction due to shellfish (crustaceans))
o T78.03 (Anaphylactic reaction due to other fish)
o T78.04 (Anaphylactic reaction due to fruits and vegetables)
o T78.05 (Anaphylactic reaction due to nuts and seeds)
• Excludes2 anaphylactic reaction due to peanuts (T78.01)
o T78.07 (Anaphylactic reaction due to milk and dairy products)
o T78.08 (Anaphylactic reaction due to eggs)
o T78.09 (Anaphylactic reaction due to other food products)
o Excludes2 food additivities allergy status (Z91.02)
o Z91.010 (Allergy to peanuts)
o Z91.011 (Allergy to milk products)
• Excludes1 lactose intolerance (E73.-)
o Z91.013 (Allergy to seafood)
o Z91.018 (Allergy to other foods (other than peanuts))