Still Stuck On Discharge Assessment Rules? 3 Scenarios Show You The Way
Remember: Don’t code ‘return anticipated’ if resident will be gone for longer than 30 days.
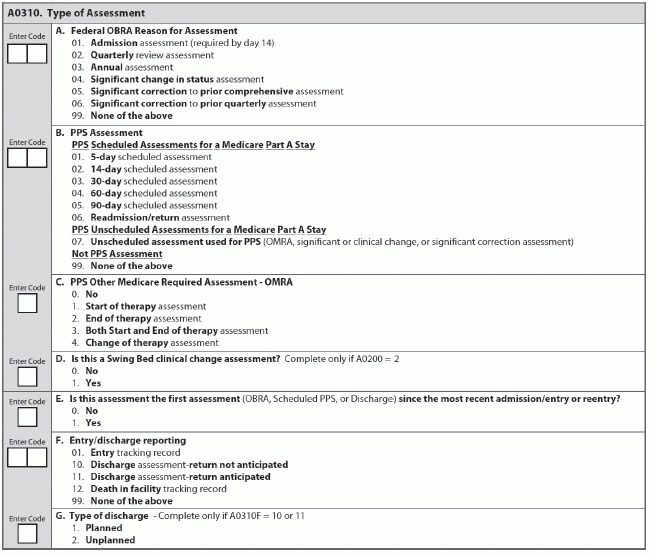
When you’re dealing with discharge assessment items under A0310 — Type of Assessment, specifically A0310F — Entry/discharge reporting and A0310G — Type of discharge, you have several options to choose from. And selecting the wrong option is often an easy mistake to make. Here are a few examples to help you understand correct discharge coding.
Example Shows You When to Code ‘Unplanned Discharge’
Scenario #1: Mrs. Green suffers what appears to be a mild stroke during lunch in the dining hall. She leaves for the hospital via ambulance and enters the emergency department to stabilize. She remains in observation for two days before returning to the nursing home.
You would code this in A0310G — Type of discharge as an “Unplanned” (2): “Acute-care transfer to a hospital or an emergency department in order to either stabilize a condition or determine if an acute-care admission is required based on emergency department evaluation.”
“Keep in mind that once the resident is admitted or is in the observation stay greater than 24 hours, that a discharge assessment is required,” said Rabia Khan, MPH, a member of the Quality Measurement and Health Assessment Group at the Centers for Medicare & Medicaid Services (CMS) Center for Clinical Standards and Quality, in a recent CMS instructional session.
How to Predict ‘Return Not Anticipated’
Scenario #2: Mr. West unexpectedly decides to transfer to an assisted living facility in a neighboring county.
This is also an unplanned discharge. “If a resident decides to complete treatment in an alternate setting and leaves the facility, this would be considered an unplanned discharge,” Khan explained.
Additionally, you would code A0310F — Entry/discharge reporting as “Discharge assessment-return not anticipated” (10): “If a resident was discharged to home or to an assisted living facility, this would be the correct type discharge to complete,” Khan said. “And in the event that the resident returned, the facility would begin the assessment process over again with an admission assessment, after completing an entry tracking record signifying that the resident is an admission.”
When ‘Return Anticipated’ & ‘Planned Discharge’ Go Hand-in-Hand
Scenario #3: Mrs. Brown leaves your facility for a hospital stay involving a scheduled knee surgery. Due to her multiple chronic health conditions, she expects to remain in the hospital for one or possibly two weeks after the surgery, and then return to the nursing home.
For this example, you would code A0310F as “Discharge assessment-return anticipated” (11) and A0310G as “Planned” (1).
“For a resident discharge to a hospital or other setting, such as a respite resident, who comes in and out of the facility on a relatively frequent basis, and reentry can be expected, the resident status is ‘Discharge, Return Anticipated,’” Khan noted. “Unless it is known on discharge that he or she will not return within 30 days.”
More: For additional information on completing discharge assessments correctly, see MDS Alert Vol. 11, No. 7, page 73, “Are You Performing Discharge Assessments Properly?”