Worried about CMPs? Know What’s Coming
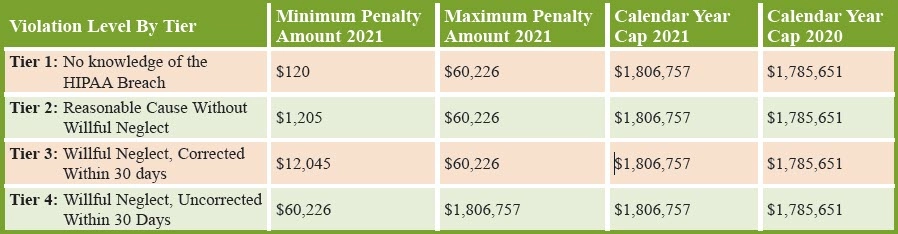
SNFs need to be extra careful about penalized noncompliance. The Centers for Medicare & Medicaid Services (CMS) has released updated specifics on the violation fines associated with civil monetary penalties (CMPs). Remember, the CMP program is designed to penalize providers, including nursing homes, that don’t comply, but can also serve as incentive for compliant nursing homes for facility-designated investment in care. Keep reading for some updates related to Health Insurance Portability and Accountability Act (HIPAA) breaches, as well as compliance issues related to nursing homes specifically. Background and Updates Definition: “A CMP is a monetary penalty the Centers for Medicare & Medicaid Services (CMS) may impose against nursing homes for either the number of days or for each instance a nursing home is not in substantial compliance with one or more Medicare and Medicaid participation requirements for long-term care facilities. A portion of CMPs collected from nursing homes are returned to the states in which CMPs are imposed. State CMP funds may be reinvested to support activities that benefit nursing home residents and that protect or improve their quality of care or quality of life,” CMS says. Update: On Nov. 15, the Department of Health and Human Services (HHS) published a final rule in the Federal Register, which adjusts amounts under HIPAA’s four-tiered penalty structure. The rule aligns with provisions previously outlined in a Sept. 6, 2016, interim final rule and also offers the mandated annual update of the amounts as codified in the Federal Civil Penalties Inflation Adjustment Act Improvements Act of 2015. Reminder: “In 2019, HHS exercised its discretionary authority and issued guidance that lowered the calendar year maximums that it would enforce to $25,000 for Tier 1 violations, $100,000 for Tier 2 violations, and $250,000 for Tier 3 violations (all subject to indexing for inflation),” explains Atlanta-based attorney Carlton Pilger with law firm Fisher & Phillips LLP in online legal analysis. The civil monetary penalty (CMP) update does show a higher annual cap amount, but “we expect OCR (Office for Civil Rights) will continue to exercise its discretion and assess the lower amounts for violations within in the first three tiers,” Pilger adds. Save This Handy Penalty Chart The HHS Office for Civil Rights (OCR) breaks down HIPAA breaches into a four-tier penalty structure. The categories range in severity and go from the lowest level, no knowledge of the HIPAA breach at Tier 1, to a more extreme breach at the highest level with the covered entity (CE) or business associate (BA) willfully ignoring and refusing to correct the breach at Tier 4. Check out this breakdown of the inflation adjustment to CMPs, which includes the 2020 Calendar Year Cap for comparison: Data for 45 CFR 160.404 from Table 1 of “Adjustment of Civil Monetary Penalties for Inflation and the Annual Civil Monetary Penalties Inflation Adjustment for 2021” final rule at www.govinfo.gov/content/pkg/FR-2021-11-15/pdf/2021-24672.pdf. Note Additional HIPAA CMP Changes The final rule also addresses other HIPAA-related penalties, too. For example, the penalty for violation of the confidentiality provision of the Patient Safety and Quality Improvement Act (PSQIA), which aims to improve patient safety by encouraging providers to identify and report medical errors, increased from $12,919 in 2020 to $13,072 in 2021. And even though the fine is small, OCR can still hit providers with CMPs for HIPAA administrative simplification violations that happened before Feb. 18, 2009, the rule suggests. That CMP amount for these HIPAA violations that occurred before that 2009 date jumped from $64 in 2020 to $162 in 2021. Use This Nursing Home CMP Refresher, Too If your facility applies for and receives CMP funding, you can use the money in several ways, all of which should help or otherwise support residents. CMS says that CMP funds can be used by nursing homes for: CMS has designed and published several toolkits for nursing homes to improve several aspects of the care they provide, by investing time and energy in those providing the care, including “Nursing Home Staff Competency Assessment,” “Nursing Home Employee Satisfaction Survey,” and “Guide to Improving Nursing Home Employee Satisfaction,” as well as a toolkit for “Head to Toe Infection Prevention.” Resource: You can find these toolkits available for download, www.cms.gov/Medicare/Provider-Enrollment-and-Certification/SurveyCertificationGenInfo/LTC-CMP-Reinvestment. Bottom line: With CMPs increasing, you should make sure your 2022 compliance planning encompasses HIPAA breaches too, specifically risk assessment and management, experts advise. Analyzing your organization’s risks pre-violation can help you cut costs down the line. Why? It’s a whole lot cheaper to nip your HIPAA risks in the bud before they become major violations that carry significant penalties. “If an organization does not do a sufficient job of addressing the rules, an incomplete compliance effort, such as ignoring repeated recommendations to reduce risks, can easily be seen as a more culpable situation,” warns Jim Sheldon-Dean, founder and director of compliance services for Lewis Creek Systems, LLC in Charlotte, Vermont. This puts “the entity into a higher penalty bracket, and the distinction[s] between penalty levels may provide a greater opportunity for HHS to reasonably use the ‘willful neglect’ levels of penalty.” Resource: Find the CMP adjustment rule, which became effective on Nov. 15, at www.govinfo.gov/content/pkg/FR-2021-11-15/pdf/2021-24672.pdf.