Code Pressure Ulcers Like This
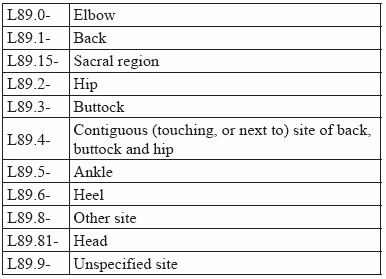
Sequence, then specify site, side, and severity for success. When residents spend a lot of time confined to a wheelchair, a chair, or a bed, they can also develop an unpleasant condition. Pressure ulcers, also called pressure injuries, can present a challenge even for the most experienced coder — and nurse assessment coordinators (NACs) have so much on their plates that they may already lack fluency in ICD-10 coding. You know that the Centers for Medicare and Medicaid Services (CMS) and state surveyors are laser-focused on reducing the incidence of pressure injuries. With the latest updates to the MDS and the RAI Manual — not to mention the coming patient-driven payment model (PDPM) system and recategorization of reimbursement — assessing pressure injuries and coding any incidence accurately will be even more important down the line. Note: While CMS has transitioned its language to better reflect that used by National Pressure Ulcer Advisory Panel (NPUAP), including prioritizing the usage of the terminology “pressure injury,” the ICD-10 manual still uses “pressure ulcer.” Because this article is focused on ICD-10 coding, you’ll see “pressure ulcer” used throughout. Step 1: Specify Associated Gangrene First Gangrene is a terrifying word, and hopefully you will never encounter the condition, but, when coding ICD-10, look first to the appropriate section and codes for that particular condition. If your colleague’s notes indicate the resident has gangrene, you’ll need to code that first before you dig into the L89 codes. ICD-10 directs you to code the condition with I96 (Gangrene, not elsewhere classified) and sequence it before the specified pressure ulcer. Step 2: Code for Site ICD-10 breaks down pressure ulcer sites in the following way. Very often, residents will present with pressure ulcers in multiple sites, which can result in a sequencing issue. When that occurs, go back through the clinical record to see, first, whether all the injuries are being treated. If there’s only one, then that’s all you’ll need to code; if there are more, you would sequence them by severity, putting the most severe first. Coders should also be aware that coding L89.89- (Pressure ulcer of other site) is not the same as coding L89.9- (Pressure ulcer of unspecified site). As Melanie Witt, RN, CPC, MA, an independent coding expert based in Guadalupita, New Mexico, explains it, “’Other site’ means that the provider has indicated where the ulcer is, but there is no specific code under L89.- that specifies the site documented.” “L89.9-,” Witt continues, “would mean that the provider has not documented where the ulcer is at all.” Coding caution: Marcella Bucknam, CPC, CCS-P, COC, CCS, CPC-P, CPC-I, CCC, COBGC, manager of clinical compliance with PeaceHealth in Vancouver, Washington, warns coders that coding L89.9- “is very rare, but use of the unlisted code is on the rise because physicians have the unspecified code as their default code choice in their EHR [electronic health records]. Using this code,” Bucknam advises, “could cause problems for treatment and care reimbursement, as certain care is more appropriate for feet as opposed to the sacrum, hips, or other locations that pressure ulcers may appear.” Step 3: Code for Laterality The L89 codes are broken down further by laterality, which means that you can choose between right, left, and unspecified anatomic areas of most sites. There are no bilateral codes, however, which means that pressure ulcers that equally affect both sides of regions such as the hips and buttocks have to be coded separately using the codes for right and left. Step 4: Code for Severity Pressure ulcers are categorized by degrees of severity, known as stages, that correlate to the depth of the tissue damage. They range from stage one, where the skin is merely inflamed and red, through to stage four, where there is bone-deep tissue loss along with necrosis. Here, again, coders can be confused by word use, as ICD-10 classifies two other stages as “unspecified” and “unstageable.” Here, unstageable simply means that the depth, or stage, of the wound cannot be determined as slough and/or eschar are covering the wound bed. As both enable the wound to heal, your provider won’t remove them to determine the stage, so the stage is classified unstageable. However, Bucknam again warns that coding a pressure ulcer as unstageable is a rare occurrence. Go above and beyond: For more details about the National Pressure Ulcer Staging System, go to https://www.ncbi.nlm.nih.gov/books/NBK2650/pdf/Bookshelf_NBK2650.pdf. Tread Carefully with Documentation Both Witt and Bucknam remind coders to keep a close eye on the documentation they are reviewing. “Pressure ulcer details, like staging,” Bucknam says, “are often documented by nurses, and coders should only use documentation provided by the physician.” Witt agrees, adding that even though nurse documentation “can be used to code the stage at this encounter, it is the provider who is attending the patient at this visit who is responsible for assigning the severity of the ulcer.”