Don't Get Tripped Up By Section H Toileting Trials
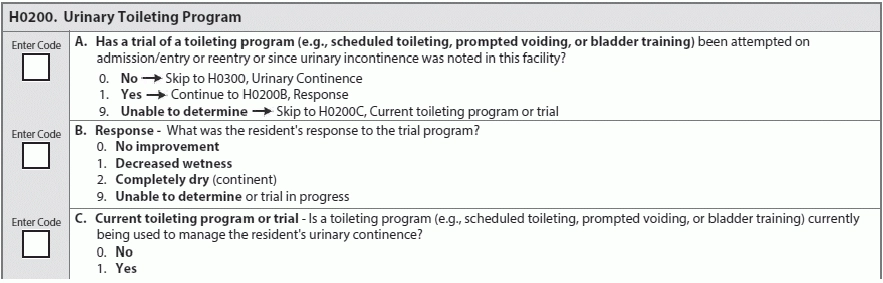
Use toilet training programs to keep residents comfortable and bolster care plans. Reevaluate your toilet training programs to stay on top of MDS sub-item H0200 (Urinary Toileting Program), as well as make sure you’re meeting Quality Measures. H0200 is also unique in the MDS because it explicitly requires establishing a personalized, individual care-plan for a resident. Learn the tricks specific to coding H0200 successfully, and then take the quiz on page 90. Familiarize Yourself With the Context An individualized toilet training program is useful for reducing or preventing incontinence in many residents, even those suffering from dementia. Your keys to success are thoroughness in your assessments and observations, as well as flexibility when implementing and modifying a resident’s program. Be thorough in your assessment of a resident’s continence level or whether she’s at risk for incontinence. When performing your assessment, examine these factors, per the RAI Manual: If a resident appears incontinent and has treatable conditions that could be causing incontinence, such as a medication change that causes intense drowsiness, treat those changeable variables first. Tip: Make sure everyone is involved, at all levels of care and administration. “One of the keys to successfully implementing a trial toileting program is ensuring that involved staff are aware of and consistently follow the established plan that was developed,” says Linda Elizaitis, president of CMSCompliance Group Inc. in Melville, New York. “Even one staff member who does not prioritize maintaining a trial toileting program can make a trial program unsuccessful — you need staff buy-in, as maintaining the structure of such a program is important for success.” Look For Past Evidence Check the resident’s clinical record for previous trials of toileting programs. A toileting program trial would include at least three days of observations on toileting and voiding, including the results. Trials may have other names, like habit training, scheduled voiding, bladder rehabilitation, or bladder retraining, the RAI Manual says. Remember: A toileting or trial toileting program is highly specific to an individual resident, and requires planning, observation, monitoring, adjustment, maintenance, and evaluation. Though staff are encouraged to track continence status, keep a resident clean and comfortable by immediately changing him out of soiled garments, and assisting a resident when toileting or hygiene, none of these constitute a proper toileting program. Hint: Don’t forget to make sure the plan is in the resident’s care plan; set your goal and interventions, says Terry Raser, Rn, RaC-Ct, Dns-Ct, QCP, senior consultant at LW Consulting inc. in Harrisburg, Pennsylvania. Re-evaluate the interventions and update them as necessary, and, most importantly, don’t forget to document the resident’s response to the program, she adds. How to Code The values for H0200A (Urinary Toileting Program, Has a trial of a toileting program … been attempted …?) are You should use 0 (No) if a resident did not undergo a toileting trial, regardless of the reason. Code 0 for continent residents, residents with a permanent catheter or ostomy, or residents who are unwilling to participate in a toileting program trial, per the RAI Manual. Use value 1 (Yes) for residents who participate in an individualized toileting program at least one time since the resident’s entry or reentry, or since incontinence was first noted. Use value 9 (Unable to confirm) if you cannot obtain records to check whether a resident has participated in a toileting program in the past. Remember: Because the lookback period for this sub-item is the most recent admission, entry, or re-entry, or since incontinence was first observed and noted in this facility, you should have the records on hand to confirm that a resident either participated or did not participate in a toileting program, so you shouldn’t have much use for value 9. The values you need to code H0200B (Urinary Toileting Program, Response) are Sub-item H0200B (Urinary Toileting Program, Response) requires you to interview and record the resident’s responses. Look for changes in the frequency and severity of wetness, per the RAI Manual. For sub-item H0200C (Urinary Toileting Program, Current toileting program or trial), use these values to code: Hint: Although the MDS description of sub-item H0200C, provides the following examples in its item description: the RAI Manual specifies that you should code: for a resident undergoing a toileting trial program. Remember: Toileting protocols qualify as a toileting program or trial program only if toileting behavior is planned, observed, maintained, adjusted (if needed), evaluated, and recorded.