Stay Current on Assessing Shortness of Breath
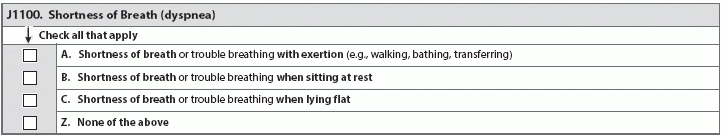
Interview, assess, observe - but what if you find conflicting information? You and team members may be inclined only to follow the RAI Manual's specific instructions for evaluating and recording a resident's shortness of breath, but effectively recording potential shortness of breath can be complicated. Shortness of breath is a serious condition that can affect almost every aspect of a resident's life, including causing distress, and contributing to the resident pulling back from activities and interaction. Shortness of breath can vastly diminish a resident's quality of life. Shortness of breath can be indicative of a change in condition, which should trigger further assessment. Adjust the resident's care plan to address any underlying illnesses that could cause or make shortness of breath worse. Note: Make sure the care plan provides for symptomatic treatment of shortness of breath, in case the cause isn't easily irreversible, according to the RAI Manual. Use these Parameters for Assessment The key to assessing residents' shortness of breath is to keep in mind what the MDS requires for coding item J1100 (Shortness of Breath). To code the J1100 correctly, you and your team need to assess whether an individual resident has shortness of breath through various body positions and activities across the seven-day lookback period. The RAI Manual says you or staff should begin assessment via interviewing the resident. Observe whether the resident seems to be experiencing any shortness of breath during the interview, and ask whether she experiences shortness of breath during any part of the day for the past seven days. The MDS specifies that staff should ask residents if they experience shortness of breath during activities requiring exertion (such as walking), as well when at rest while sitting, and while lying flat. "Residents who have those problems - especially J1100A (... with exertion) and J1100B (... when sitting at rest) - are usually fairly easy to hear, see, and observe," says Jane Belt, Ms, Rn, RaC-Mt, QCP, curriculum development specialist at American association of nurse assessment Coordination (AANAC), in Denver. Keep in mind: Some residents won't want to tell staffthat they're experiencing shortness of breath, and may go through some lengths to try and hide the symptom. The RAI Manual warns of residents adjusting their beds so the head is elevated and their discomfort is alleviated, and still not mentioning the symptom to staff. "J1100C (... when lying flat) is the trickier one since often the resident makes the adjustment themselves - raises the head of the bed, uses an extra pillow or two," Belt says. "Part of the MDS data collection is observing that resident and talking to the resident - most will usually tell you why they are using a pillow or the head of the bed is usually elevated, but you have to observe and ask the questions!" The RAI Manual lists these signs of shortened breath or trouble breathing: "Increased respiratory rate, pursed lip breathing, a prolonged expiratory phase, audible respirations and gasping for air at rest, interrupted speech pattern (only able to say a few words before taking a breath) and use of shoulder and other accessory muscles to breathe." If you observe any of these signs, make sure to note the activity or body position in which the resident experienced the shortness of breath. "Plus, the shortness of breath item is not actually an interview so it takes assessment and observation skills. There are things to observe, like skin color, counting respirations, listening to lung sounds - which all make great times to talk to the residents about their breathing," Belt says. Because residents may try to downplay the intensity or existence of their symptoms, you and your team may need to weigh your own observations, as well as the clinical record and input from the resident's representative or family, against what residents tell you. Though person-centered care relies on putting the resident at the center of her own care and taking her at her word, the RAI Manual emphasizes the importance of accurately assessing and recording any shortness of breath - and finding out the cause. "Then part of the nursing process would be to take those findings from observation and ask appropriate questions if the resident is able to understand. Again - how does the nurse phrase the question - shortness of breath or trouble breathing. Most residents are going to understand trouble breathing rather than thinking about shortness of breath," Belt says. Interview team members across all shifts, and talk to the resident's representative or family to find out if the resident has ever had a history of shortness of breath. Remember: Allergies and other environmental factors may exacerbate trouble breathing at certain times of the year, especially if your facility is in a geographic location that experiences seasons. Record and code all shortness of breath, even if the resident personally attributes the symptoms to seasonal allergies or other known environmental factors. If the resident experiences shortness of breath during exertion and also at rest, make sure you code J1100 (Shortness of Breath) by checking each sub-item that the resident experiences during the seven-day lookback period. Note: Residents may feel such discomfort from their shortness of breath that they avoid activities or interaction. Take these avoidance strategies into account when deciding how to code J1100 (Shortness of Breath). If the resident does not claim to experience shortness of breath, and neither you nor your team members can find any suggestion or evidence of shortness of breath from your observations or the clinical record, nor input from family or the resident representative, then you would code J1100 by checking Z (None of the above).