Understand Drug Regimen Review Expansions
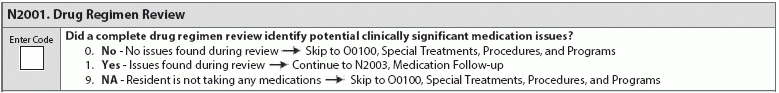
Don’t fall prey to the trickiness of new requirements for drug review. Like so many aspects of care, documentation is everything in conducting a watertight Drug Regimen Review (DRR) and filling out MDS item N2001 (Drug Regimen Review) with the most accuracy possible. What has changed? Basically, the DRR expansion means that the resident’s clinical record must be looked over and taken into account. “The requirements for the Drug Regimen Review (DRR) have been expanded for nursing homes under the updated Requirements of Participation. While the consultant pharmacist has always had to conduct a monthly review for each resident, the review must now include a review of the resident’s medical chart. It also expands upon the required reporting of irregularities, which includes relatively common issues such as use of meds without appropriate indication, without adequate monitoring, or in excessive doses,” says Linda Elizaitis, RN, BS, RAC-CT, CIC, president and CEO of CMS Compliance Group in Melville, New York. Who needs to be involved? You won’t be surprised to know that reviewing drug regimens falls to consultant pharmacists, but at least three other people need to be involved in the drug review, too, if the pharmacists find irregularities. “First, the regulations require that a separate written report must be sent to the attending physician, director of nursing and also the medical director that outlines any irregularities identified by the pharmacist. Second, the attending physician is required to document in the medical record that the irregularity has been reviewed, and what actions have been taken, if any. If the attending disagrees with the recommendation, he needs to document a clinical rationale, not just state that he disagrees with the recommendation,” she says. Prepare for survey or risk extra scrutiny While you prepare for a survey, take stock of which residents need an initial or updated MDS. “During survey, providers are required to fill out a matrix for newly admitted residents who haven’t had an MDS completed yet, as well as for all other residents. One of the areas of the matrix that must be filled out relates to medications, so residents receiving any of a list of ‘high-risk’ meds will be identified ahead of surveyors selecting the survey sample. These medications include insulin, anticoagulants, antibiotics, diuretics, opioids, hypnotics, anti-anxiety, antipsychotic, antidepressant and/or respiratory meds,” Elizaitis says. There is good news, as this information is needed for another item in the MDS. But remember, surveyors are already on the lookout for this information, so accuracy must be a top priority. “This listing of meds probably looks familiar to those who work with the MDS because the majority of this list is required to be coded under N0410 Medications Received (with the exception of insulin and respiratory meds). Providing this information to surveyors could potentially increase the likelihood that a resident is added to the survey sample, which will then lead the surveyors to look at the accuracy of the MDS and if the MDS accurately reflects the residents’ medical record information,” Elizaitis says. Prepare for October updates The upcoming changes to Section N in the MDS should prompt you to take a good look at your facility’s drug regimen review process. “The addition of the three new items in Section N Medications for the October 1, 2018, version of the MDS indicates the emphasis that CMS has placed not only on the review of each resident’s drug regimen, but the associated communication and actions taken if issues are identified. N2001 asks if a complete drug regimen review identified potential clinically significant medication issues,” Elizaitis says. Top tip: Make sure you and team members, especially those involved in the drug regimen review, fully understand “clinically significant” and are on the same page. “Clinically significant issues, defined in Appendix PP of the State Operations Manual, are ‘effects, results or consequences that materially affect or are likely to affect an individual’s mental, physical or psychosocial well-being either positively by preventing, stabilizing, or improving a condition or reducing a risk, or negatively by exacerbating, causing or contributing to a symptom, illness or decline in status,” Elizaitis says. Know what to do if these coding situations arise; your responsibilities go beyond filling out the MDS here. “If these types of issues were identified, the coder is directed to N2003, which asks if the facility contacted a physician ‘by midnight of the next calendar day’ and completed the physician’s recommended actions to address the identified problems. N2005, the third new item, looks at medication intervention and whether the facility notified the physician timely and took action each time there were issues identified since the resident’s admission,” Elizaitis says. Surveyors are looking for both for accountability and making sure that facility teams are communicating across specialties and roles. Documentation is, as usual, crucial to providing evidence to surveyors, particularly, that everything is in good working order, in both facility communication and execution. “This means that facilities need to ensure that any clinically significant irregularities that are identified by the consultant pharmacist are not only acknowledged timely by the physician but acted upon quickly as well. If issues are identified, they need to be quickly addressed, and, if indicated, an ad-hoc [Quality Assurance] QA Committee meeting should be considered to review and identify any other potentially at-risk residents who may be receiving a similar drug(s) to ensure its use is appropriate. Additionally, the importance of documentation related to what updates to the care plan and resident’s medications were made cannot be understated in correcting identified issues,” Elizaitis says. Review roles and responsibilities, too The updates to Section N, the drug regimen review particularly, and the survey process more generally all emphasize a need for facilities to respond quickly. Now is a great time to review team member responsibilities and roles so everyone knows who is responsible for what before an issue arises — and can respond to and resolve any findings as quickly as possible. “Lastly, when reviewing your policies and procedures related to drug regimen reviews and follow-up, be clear as to what the physicians’ and nurses’ responsibilities are, as well as what protocol is to be used if the consultant pharmacist identifies a significant concern. It will not be acceptable to simply wait for the physician to respond to such a finding weeks or even days later. Make sure that you spell out what communication mechanisms is to be used by the consultant pharmacist to alert the physician, medical director and director of nursing of any significant medication issue,” Elizaitis says.