Make Sure You're Correctly Dealing With SCSA Matters For Hospice Care
Pay attention to timing issues to anticipate when you don’t need to do an SCSA.
There are a whole host of guidelines in the RAI Manual for completing a Significant Change in Status Assessment (SCSA), and that means it’s pretty easy to make a mistake. Understanding when you must (versus when you don’t need to) complete an SCSA for hospice care-related changes is even trickier at times. Here’s what you need to know to sort this all out.
Did You Miss This Important MDS Update?
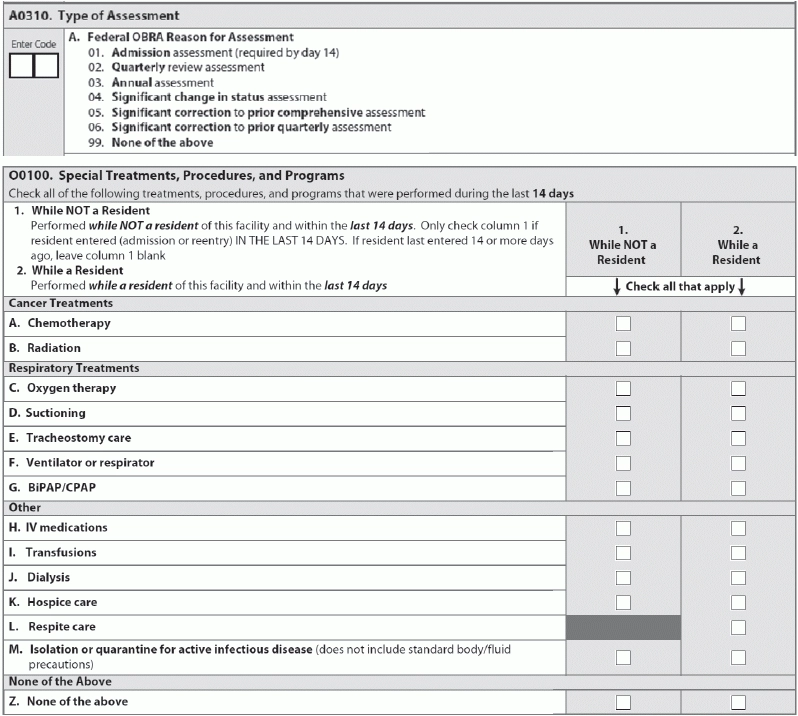
In the last RAI Manual update (October 2015), the Centers for Medicare & Medicaid Services (CMS) updated its instructions regarding the SCSA for hospice (item O0100K — Hospice care). The new instructions state that in addition to completing an SCSA when a resident revokes or initiates hospice care, you must also complete an SCSA if a resident changes hospice providers.
Problem: But some people missed the rule change and don’t know that that they need to complete an SCSA when the resident switches hospice providers, says Michelle Synakowksi, LNHA, RN, C-NE, RAC-MT, Director of ProCare and a consultant at Leading Age New York.
CMS found that when residents changed hospice providers, care coordination would sometimes fall through the cracks, Synakowski explains. So requiring you to complete an SCSA when residents switch hospice agencies gives you an opportunity to review the care plan. This requirement also prompts you to coordinate with the hospice provider so you know what services the hospice is providing and what service your facility is providing for the resident.
Make Sure You’re Following These Rules
Prior to the October 2015 update, “the rule was you had to do an SCSA if initiated on hospice or discontinued hospice,” Synakowski states. This hasn’t changed.
You must complete an SCSA when a resident enrolls in a hospice program (Medicare-certified or State-licensed hospice provider), according to Scott Heichel, RN, RAC-CT, DNS-CT, Director of Clinical Reimbursement at LeaderStat (www.leaderstat.com). “The assessment reference date (ARD) must be within 14 days from the effective date of the hospice election.” And you must perform an SCSA regardless of whether you recently conducted an assessment on the resident.
Also, an SCSA is required “when a resident is receiving hospice services and then decides to discontinue or revoke those services,” Heichel notes. In this case, the ARD must be within 14 days from one of the following:
1. The effective date of the hospice election revocation;
Keep an Eye on the ARD
But there are a few situations that you need to keep in mind. Regarding exceptions to the rule of completing an SCSA when revoking or initiating hospice care, “it’s really a timing issue,” Synakowski notes.
“Often the Admission assessment is the most confusing time for MDS nurses related to a resident’s hospice status and determining the need for an SCSA,” says Judi Kulus, MSN, MAT, RN, NHA, RAC-MT, DNS-CT, QCP, VP of Curriculum Development at the American Association of Nurse Assessment Coordination (AANAC). “The resident might come into the facility with hospice orders and may decide to go off hospice, or the opposite might occur.”
Case in point: You don’t need to complete an SCSA if the resident is admitted to your facility already on the hospice benefit or elects hospice on or prior to the ARD of the Admission MDS, Heichel instructs. You should check item O0100K on the Admission assessment, but “since the hospice election was already captured on the Admission MDS, completing an SCSA is not required.”
Another scenario is when the hospice election occurs after the Admission assessment ARD but prior to its completion, according to Heichel. In this case, “facilities may choose to adjust the ARD to the date of hospice election so that only the Admission assessment is required.”
Example: A few days after a resident is admitted on regular rehab PPS coverage, the family says that they want hospice care, Synakowski illustrates. Because the hospice initiation occurs prior to the ARD, you’ll capture the hospice in the Admission assessment.
Don’t Be Afraid to Move the ARD
For revoking hospice care, you nearly always have to complete an SCSA, according to Synakowski. The only exception is when the Admission assessment captures the hospice status, meaning the resident revoked hospice before the ARD and you were able to reflect that on the Admission MDS. In this case, you don’t need to do an SCSA.
Also, when the resident revokes hospice care after the Admission assessment ARD but prior to your completing the Admission assessment, CMS allows you to choose to adjust the ARD to the date of hospice revocation, so that you only need to submit the Admission assessment and not also the SCSA.
Rule of thumb: You should ask yourself whether you can move the Admission assessment ARD and set it to capture the election, revocation, or change in hospice, Kulus advises. “If yes, then only the Admission assessment is required and no SCSA needs to be scheduled after the Admission assessment.”
“Be prepared to move the Admission ARD if necessary. If the resident’s status changes during the early days of admission, then the last status on the ARD must be the focus of the CAAs and care planning process,” Kulus says. “The only way to avoid completing an SCSA shortly after an Admission assessment is to move the ARD to capture the change in hospice status. If the hospice status changes after the ARD, then an SCSA must be scheduled.”
Don’t Treat Palliative Care Like Hospice
Mistake: Another common point of confusion is for palliative or “terminal” care versus hospice, Synakowski points out. If someone is terminal or elects palliative care but doesn’t elect hospice, this doesn’t mean you need to do an SCSA.
Instead, you would develop the care plan with goals for palliative care and all care plan approaches anticipating a decline. But you don’t automatically need to complete an SCSA.
Still, you need to determine whether the resident with a terminal condition has a change in that condition that is “an expected, well-defined part of the disease course and is consequently being addressed as part of the overall plan of care for the individual,” Heichel notes. “If a terminally ill resident experiences a new onset of symptoms or a condition that is not part of the expected course of deterioration and the criteria are met for an SCSA, an SCSA is required.”
Important: Also, make sure that the MDS completion date (item Z0500B) is no later than 14 days from the ARD (ARD + 14 calendar days) and no later than 14 days after the determination that the resident’s situation has met the criteria for an SCSA, Heichel stresses. “This date may be earlier than or the same as the Care Area Assessment (CAA) completion date, but not later than.”
Best bet: If you run into situations involving hospice and are unsure of whether you need to complete an SCSA, always refer to the RAI Manual. You can find SCSA-related information in Chapter 2, section 2.5, Assessment Types and Definitions (starting on page 2-7), and section 2.6, Required OBRA Assessments for the MDS (starting on page 2-14).
2. The expiration date of the certification of terminal illness; or
3. The date of the physician’s or medical director’s order stating the resident is no longer terminally ill.