4 Ways You Might Be Wrecking Your K0510 Coding
Hint: Your biggest battle may lie with K0510D Therapeutic diet.
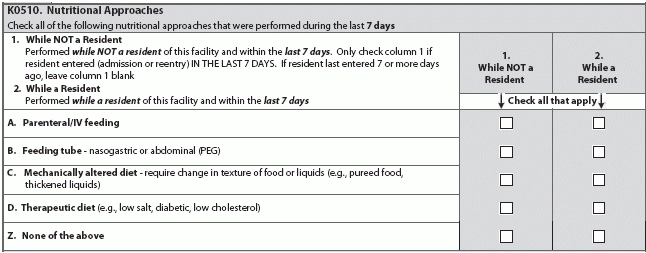
The K0510 Nutritional Approaches section of the MDS gives you the opportunity to record all approaches in the past seven days both inside and outside your facility. But each of the Nutritional Approaches items can trip you up, causing glaring mistakes in your MDS coding. Here are the four of the most common mistakes.
1. K0510A: Don’t Code Fluids for Medication Administration
Coding all IV fluids for K0510A Parenteral/IV feeding might be tempting, but beware of coding any fluids that you are not giving to meet nutrition or hydration needs. For example, you can’t code K0510A for IV fluid given solely to administer a medication, according to a recent Pennsylvania Department of Health
Example: A resident goes to the ER with a UTI diagnosis, and is given IVs for medication administration and to establish vascular access. In this case, you would not code this for K0510A unless the ER staff gave the resident IV fluids for hydration and not just as a medication administration vehicle, PA-DOH explained.
Bottom line: To code K0510A, whatever is administered must be done so for nutrition and hydration purposes, according to a recent presentation by Barbara Thomsen, CDM, CFPP, RAC-CT, Iowa’s MDS/OASIS Automation Coordinator with the Iowa Foundation for Medical Care/Telligen in West Des Moines.
2. Understand ‘Mechanically Altered’ Vs. ‘Therapeutic’
According to the RAI Manual, the definition for K0510C “mechanically altered” diet is “a diet specifically prepared to alter the consistency of food in order to facilitate oral intake; examples include soft solids, pureed foods, ground meat and thickened liquids.”
In contrast, the definition for K0510D “therapeutic diet” is “a diet intervention ordered by a health care practitioner as part of the treatment for a disease or clinical condition manifesting an altered nutritional status, to eliminate, decrease or increase certain substances in the diet (e.g., sodium, potassium).”
What’s often confusing is how these RAI Manual definitions differ from the definition for therapeutic diet under F325, PA-DOH noted. The F325 definition actually combines both mechanically altered food and the therapeutic diet definition from the RAI Manual.
What to do: For MDS 3.0 coding, don’t code a mechanically altered diet as therapeutic unless it also meets the K0510D definition, regardless of the F325 definition, PA-DOH explained. “Be sure when you are talking with surveyors that everyone is clear as to how the phrase ‘therapeutic diet’ is being used.”
Remember: You don’t define a therapeutic diet by the “content of what is provided or when it is served, but why the diet is required,” the RAI Manual guidance states. “Therapeutic diets provide the corresponding treatment that addresses a particular disease or clinical condition which is manifesting an altered nutritional status.”
Also, be sure you’re coding enternal feeding formulas as K0510D when the formula is altered to manage problematic health conditions, such as enternal formulas specific to diabetics, Thomsen noted. You should not code enternal feeding formulas as K0510C Mechanically altered diet.
3. Don’t Second-Guess K0510B Coding
Unlike K0510A Parenteral/IV feeding, you would code K0510B Feeding tube regardless of whether you’re actually using the tube for nutrition or hydration purposes. “Just the presence of the tube is sufficient for coding this item,” PA-DOH explained.
According to the MDS 3.0, the definition for K0510B Feeding tube is: “Presence of any type of tube that can deliver food/nutritional substances/fluids/medications directly into the gastrointestinal system. Examples include, but are not limited to, nasogastric tubes, gastrostomy tubes, jejunostomy tubes, percutaneous endoscopic gastrotomy (PEG) tubes.”
Example: A resident has a G-tube, and it’s kept patent with flushes but isn’t being used for nutrition or hydration. In this case, you can still record this for K0510B.
4. Beware of Supplements
Don’t be tempted to code dietary supplements as K0510D Therapeutic diet. Although residents may take supplements to support calorie or protein malnutrition, or for a host of other health reasons, you can’t code K0510D if the supplements aren’t treating a specific disease or condition.
“Alone, supplements do not constitute a therapeutic diet; they must be administered as part of a therapeutic diet to manage problematic health conditions,” PA-DOH said.
Example: A resident is on a supplement due to poor appetite with no related diagnosis. In this case, you would not code K0510D.
Another Example: The physician orders a regular diet with protein supplements to aid in healing a resident’s pressure ulcer. In this case, you would code K0510D only if the protein supplements are also helping to treat a specific protein deficiency, PA-DOH stated.
“Nutrition interventions implemented as part of a treatment plan for a clinical condition (such as pressure ulcers) may be therapeutic, but don’t necessarily meet the definition of a therapeutic diet,” PA-DOH clarified. Conversely, if a resident takes a protein supplement as part of a therapeutic diet to treat low albumen, you have an identified specific deficiency and you can code K0510D.
(PA-DOH) training teleconference Q&A session.