What 'Present On Admission' Really Means
Learn how to apply for the On-Time Pressure Ulcer Prevention Program.
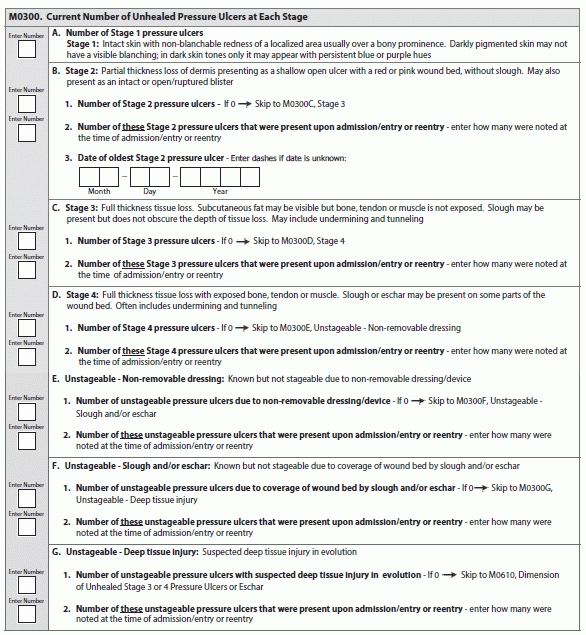
Coding Item M0300 — Current Number of Unhealed Pressure Ulcers at Each Stage can be tricky at the best of times. But when you need to determine whether a pressure ulcer was present at the time of admission/entry or reentry, you have an even thornier task at hand — particularly when the resident leaves and then reenters the facility.
‘Present on Admission’ Isn’t as Straightforward as it Seems
So when is a pressure ulcer “present on admission?” What if the resident leaves your facility and returns within 30 days with the same pressure ulcer at the same stage? The Centers for Medicare & Medicaid Services (CMS) recently issued a clarification to answer this question.
Example: Mr. Smith leaves your facility for a hospital stay. When he left your facility, he had a Stage 2 pressure ulcer on his left buttock. He returns to your facility 12 days later and still has the same Stage 2 pressure ulcer; this pressure ulcer hasn’t worsened, nor has it gotten any better.
Upon Mr. Smith’s return to your facility, should you code this pressure ulcer as present on admission? Thankfully, the RAI Manual (Chapter 3, page M-7) provides instructions for determining whether a pressure ulcer was present on admission, according to a Dec. 30, 2015 provider alert from the Texas Department of Aging and Disability Services (DADS).
“For each pressure ulcer, determine if the pressure ulcer was present at the time of admission/entry or reentry and not acquired while the resident was in the care of the nursing home,” the RAI Manual states. “Consider current and historical levels of tissue involvement.”
Understand the Rationale
The RAI Manual explicitly states that if a resident who has a pressure ulcer is hospitalized and returns with that pressure ulcer at the same numerical stage, you should not code the pressure ulcer as “present on admission.” Why? The RAI Manual’s reasoning for this coding instruction is because the pressure ulcer was present at the facility prior to the hospitalization.
Meaning: If the resident was admitted to your facility, was subsequently transferred to the hospital with the same pressure ulcer at the same stage as it was at the time of admission, and then returned to your facility with that same pressure ulcer at the same stage, you would code it as “present on admission” in Item M0300. This is because the resident did not acquire the pressure ulcer while in the care of the nursing home staff, DADS noted.
Also, if the pressure ulcer was not “present on admission” when nursing home staff identified it, or if a pressure ulcer that was “present on admission” increased in stage while receiving nursing home care, you would not code it as “present on admission” when the resident returned from the hospital with the ulcer at the same stage as it was when he left, DADS explained. “This is because the ulcer was either acquired or worsened to a higher stage while under the care of nursing home staff.”
Coded Incorrectly? Here are Your Next Steps
If the pressure ulcer was present on admission/entry or reentry and then increased in numerical stage during the resident’s stay, you would code that pressure ulcer at the higher stage — but don’t consider that higher stage as “present on admission.” And if a current pressure ulcer increases in numerical stage during a hospitalization, you must code that ulcer at the higher stage upon reentry and code it as “present on admission.”
If the pressure ulcer was unstageable on admission/entry or reentry but becomes numerically stageable later, you would consider it “present on admission” at the stage at which it first becomes numerically stageable. But if that pressure ulcer then subsequently increases in numerical stage, you would not consider that higher stage as “present on admission.”
What to do: You should correct all MDS records that were not appropriately coded in this fiscal year (since Oct. 1, 2015) within 14 days of this clarification and note the error, DADS instructed. “Modifications to correct the errors must be made, even though there will be no impact on the Resource Utilization Group (RUG) used for payment and no impact on nursing home quality measures.”
Learn Strategies to Improve Your Pressure Ulcer Prevention
Also, if you’re looking for new and innovative ways to prevent pressure ulcers in your facility, the Agency for Healthcare Research and Quality (AHRQ) has launched a new initiative, entitled the On-Time Pressure Ulcer Prevention Program (OTPP). The AHRQ has contracted with the University of Chicago, along with its partner Stratis Health, to help 50 selected nursing homes implement and evaluate the OTPP.
The OTPP will begin in March 2016 and run for 12 months, according to a Dec. 17 alert from Washington, D.C.-based Leading Age. The selected 50 nursing homes may participate in the OTPP only if they use electronic health records (EHRs). The OTTP integrates clinical reports from a nursing home’s EHR into an evidence-based process that identifies residents who are at risk for developing pressure ulcers.
The participating nursing homes can use these reports and work with an experienced facilitator to implement team-based strategies to improve risk identification and care planning, Leading Age said. The program has already been effective in New York nursing homes, which reaped a 59-percent reduction in incidence of pressure ulcers after integrating at least three OTPP reports into the care planning process.
Link: For more information on the OTPP, go to www.ahrq.gov/professionals/systems/long-term-care/resources/ontime/pruprev/index.html.