Get Ready To Report On 3 New PAC Cross-Setting Quality Measures
Function measure spurs brand-new MDS section, too.
Since last year, the Centers for Medicare & Medicaid Services (CMS) has been promising that post-acute care (PAC) providers will soon see standardized quality measures that will require reporting across settings — and now your wait is over. You have three new uniform quality measures upon which you’ll soon need to report.
Background: The Improving Medicare Post-Acute Care Transformation (IMPACT) Act enacted on Oct. 6, 2014 called for the development of standardized quality measures for which PAC providers could all report. The quality measures would require PACs to submit standardized patient assessment data in several domains, including incidence of major falls, skin integrity, and function.
Start Reporting on 3 New Quality Measures Next Year
As part of the fiscal year (FY) 2016 SNF PPS Final Rule, nursing facilities now have the following three new measures under the SNF Quality Reporting Program (QRP):
1. “Application of Percent of Long-Term Care Hospital Patients with an Admission and Discharge Functional Assessment and a Care Plan That Addresses Function” (NQF #2631);
2. “Percent of Residents or Patients with Pressure Ulcers That Are New or Worsened” (NQF #0678); and
3. “Application of Percent of Residents Experiencing One or More Falls with Major Injury” (NQF #0674).
According to CMS, the data collection timeframe for these three new measures is Oct. 1, 2016 through Dec. 31, 2016. Your data submission deadline is May 15, 2017.
Remember: You have a lot at stake if you don’t report on these quality measures. If you fail to submit the required quality reporting data to CMS beginning in FY 2018, you’ll see a 2-percent reduction to your market basket percentage.
1. Function: New MDS Items Affect Both Quality & Coding
This cross-setting quality measure reflects the percent of residents with an admission and discharge functional assessment and a treatment goal that addresses function. The treatment goal provides evidence that you’ve established a care plan with a goal for the resident.
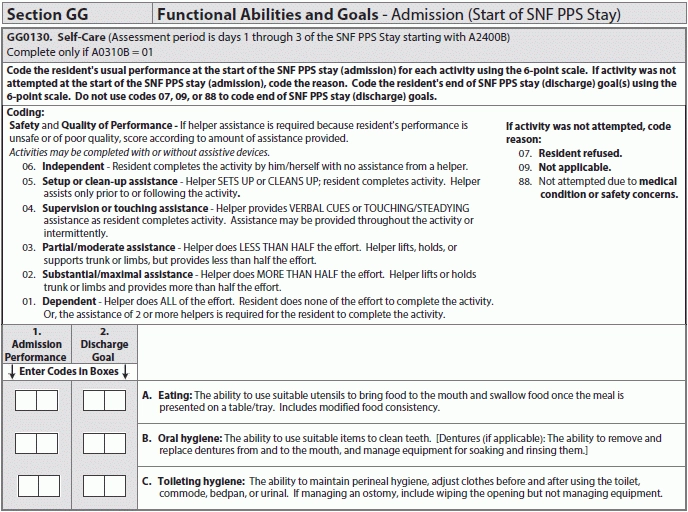
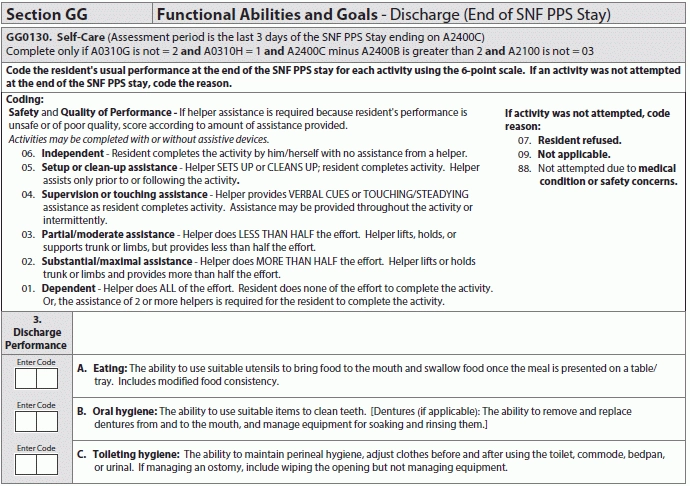
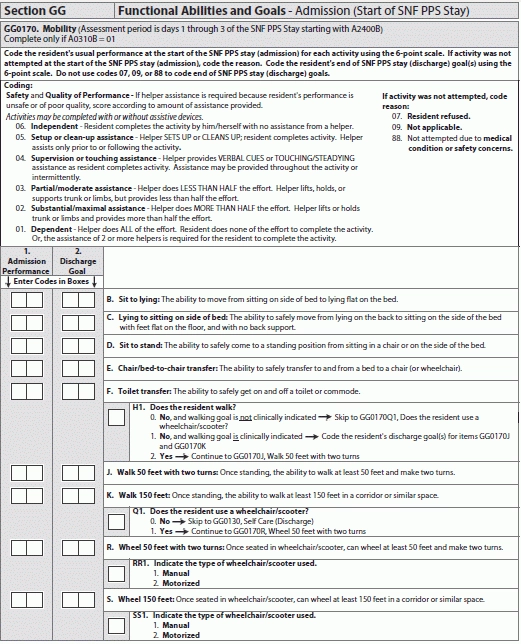
For SNFs, the quality measure is calculated using MDS 3.0 assessment data. CMS has created a new section in the MDS relating to the function quality category: Section GG — Functional Abilities and Goals, and this new section is effective Oct. 1, 2016.
The denominator for SNFs is the number of Medicare Part A covered resident stays. The numerator is the number of resident stays with functional assessment data for each self-care and mobility activity and at least one self-care or mobility goal.
Caveat: Although patients with both complete and incomplete stays are included in the numerator for this quality measure, those with an incomplete stay do not require discharge functional status data. Admission functional status data and at least one treatment goal is still required for residents with an incomplete stay, however.
Section GG is divided into two major items, one for self-care and one for mobility. Further, you must complete these items both at admission (start of SNF PPS stay) and at discharge (end of SNF PPS stay). (For more on coding Section GG, see “How To Code New MDS Section GG Items — A Primer” starting on the cover page.)
2. Skin Integrity: Focus on New or Worsening Pressure Ulcers
Specifically, this measure reports the percent of short-stay SNF residents with Stage 2 through 4 pressure ulcers that are new or worsened since admission. The measure captures all assessments during an episode of care for reports of Stage 2 through 4 pressure ulcers that were not present or were at a lesser stage since admission.
Note: For SNFs, the pressure ulcer measure will reflect only short-stay residents — those who have accumulated 100 or fewer days in the facility as of the end of the measure time window.
For the calculation, the denominator is the number of short-stay residents with one or more MDS 3.0 assessments that are eligible for a look-back scan. A look-back scan is a review of all qualifying assessments within the resident’s current episode to determine whether events occurred during the look-back period.
Certain residents are excluded from the denominator, including:
The numerator is the number of short-stay residents with an MDS 3.0 assessment during the selected time window who have one or more Stage 2 through 4 pressure ulcers that are new or worsened, based on examination of all assessments in the resident’s episode for reports of Stage 2 through 4 pressure ulcers that were not present or were at a lesser stage on prior assessment.
These include the following pressure ulcer coding in Item M0800 — Worsening in Pressure Ulcer Status Since Prior Assessment (OBRA or Scheduled PPS) or Last Admission/Entry or Reentry:
1. M0800A — Stage 2 is greater than zero (0); OR
2. M0800B — Stage 3 is greater than zero (0); OR
3. M0800C — Stage 4 is greater than zero (0).
This quality measure calculates data on a quarterly basis using a rolling six months of data. If you have residents with multiple care episodes during the six-month period, the measure will count only the latest episode. For some other residents with longer care episodes, the measure may have an extended time window of up to 100 days and may extend into the prior measurement period.
Watch out: This measure also includes certain “covariates” for risk adjustment. Certain coding in the MDS could affect the pressure ulcer quality measure, aside from the Section M items; these include:
1. Requiring limited or more assistance in bed mobility self-performance dependence on the initial assessment (if you code Item G0110A1 — Bed mobility, self-performance as: 2 — Supervision; 3 — Limited assistance; 4 — Total dependence; 7 — Activity occurred only once or twice; or 8 — Activity did notoccur).
2. Experiencing bowel incontinence at least occasionally on the initial assessment (if you code Item H0400 — Bowel Continence as: 1 — Occasionally incontinent; 2 — Frequently incontinent; or 3 — Always incontinent).
3. Having diabetes or peripheral vascular disease on the initial assessment (if you check Item I0900 — Peripheral Vascular Disease (PVD) or Peripheral Arterial Disease (PAD) in the last seven days, or Item I2900 — Diabetes Mellitus (DM) in the last seven days).
4. Having a low Body Mass Index (BMI), based on height and weight on the initial assessment (if you coding K0200A — Height and K0200B — Weight results in a BMI that is greater than or equal to 12.0 and less than or equal to 19.0).
3. Major Falls: Focus on Your J1900C Coding
The measure addresses the percentage of residents who experience one or more falls with major injury (defined as bone fractures, joint dislocations, closed head injuries with altered consciousness, or subdural hematoma) during the SNF stay.
The data for this quality measure comes from MDS Item J1800 — Any Falls Since Admission/Entry or Reentry or Prior Assessment (OBRA or Scheduled PPS), whichever is more recent. If you code 1 — Yes for J1800, you would continue to Item J1900 — Number of Falls Since Admission/Entry or Reentry or Prior Assessment (OBRA or Scheduled PPS), whichever is more recent.
For Item J1900, you can code the number of occurrences for three sub-items: J1900A — No injury; J1900B — Injury (except major); or J1900C — Major injury.
This measure reflects the data from your coding specifically for J1900C (for more on coding falls in Item J1900, see “Dig Deeper: Improve Your J1900 Coding To Avoid Quality Reporting Snafus” on page 94).
For SNFs, the denominator for the falls measure is the number of stays in the selected time window for residents with a PPS Part A Discharge Assessment (A0310H = 1). A resident stay is excluded from the denominator if none of the assessments in the look-back scan has a usable response indicating the presence of a fall with major injury during the selected time window — specifically, if all assessments have missing coding for falls with major injury (J1900C = [-]).
The numerator is the number of Medicare Part A covered resident stays where the resident experienced one or more falls that resulted in major injury.
Although only the data on the number of falls resulting in major injury (J1900C) are included to calculate this measure, the collected data for the falls measure includes all coding in both Items J1800 and J1900.
Resources: You can find several documents relating to the new quality measures and the new MDS 3.0 items posted on the CMS website: