Look For Changes Both Big & Small Sprinkled Throughout The MDS
Enjoy a third K0710 example to guide your MDS coding.
Section A wasn’t the only part of the MDS that received significant changes in the RAI manual update released on Sept. 15. The Centers for Medicare & Medicaid Services (CMS) had much more in store for other MDS sections, so pay close attention to these important revisions to Sections E, G, J, K, M, and N.
Manual Update Tweaks Wording in Section E
CMS revised two areas in Section E — Behavior. For Item E0100 — Potential Indicators of Psychosis, CMS revised the Rationale section for Example #3 to read: “The resident reports auditory and visual sensations that occur in the absence of any external stimulus. Therefore, this is a hallucination.”
For Item E1100 — Change in Behavior or Other Symptoms, Example #1 now reads:
“1. On the prior assessment, the resident was reported to wander on 4 out of 7 days. Because of elopement, the behavior placed the resident at significant risk of getting to a dangerous place. On the current assessment, the resident was found to wander on the unit 2 of the last 7 days but has not attempted to exit the unit. Because the resident is no longer attempting to exit the unit, she is at decreased risk for elopement and getting to a dangerous place. However, the resident is now wandering into the rooms of other residents, intruding on their privacy. This requires occasional redirection by staff.”
Note Helpful Definitions Now in Section G
CMS has added “Activities of Daily Living Definitions” for Item G0110 — Activities of Daily Living (ADL) Assistance on pages G-3 and G-4. Although the definitions did not actually change, previous manuals did not include them here. This section reads as follows:
A. Bed mobility: how resident moves to and from lying position, turns side to side, and positions body while in bed or alternate sleep furniture.
B. Transfer: how resident moves between surfaces including to or from: bed, chair, wheelchair, standing position (excludes to/from bath/toilet).
C. Walk in room: how resident walks between locations in his/her room.
D. Walk in corridor: how resident walks in corridor on unit.
E. Locomotion on unit: how resident moves between location in his/her room and adjacent corridor on same floor. If in wheelchair, self-sufficiency once in chair.
F. Locomotion off unit: how resident moves to and returns from off-unit locations (e.g., areas set aside for dining, activities or treatments). If facility has only one floor, how resident moves to and from distant areas on the floor. If in wheelchair, self-sufficiency once in chair.
G. Dressing: how resident puts on, fastens and takes off all items of clothing, including donning/removing a prosthesis or TED hose. Dressing includes putting on and changing pajamas and housedresses.
H. Eating: how resident eats and drinks, regardless of skill. Do not include eating/drinking during medication pass. Includes intake of nourishment by other means (e.g., tube feeding, total parenteral nutrition, IV fluids administered for nutrition or hydration).
I. Toilet use: how resident uses the toilet room, commode, bedpan, or urinal; transfers on/off toilet; cleanses self after elimination; changes pad; manages ostomy or catheter; and adjusts clothes. Do not include emptying of bedpan, urinal, bedside commode, catheter bag or ostomy bag.
J. Personal hygiene: how resident maintains personal hygiene, including combing hair, brushing teeth, shaving, applying makeup, washing/drying face and hands (excludes baths and showers).
Also for Item G0110, CMS revised the Rationale for Example #2 of G0110J — Personal Hygiene, which appears on page G-20:
“Rationale: A staff member had to complete part of the activity of personal hygiene for the resident 3 out of 7 days during the look-back period. The assistance, although non-weight-bearing, is considered full staff performance of the personal hygiene sub-task of brushing and styling her hair. Because this ADL sub-task was completed for the resident 3 times, but not every time during the last 7 days, it qualifies under the second criterion of the extensive assistance definition.”
‘Alternative Medicine’ Added to Non-Medication Pain Intervention
CMS also revised the definition of Non-Medication Pain Intervention used on page J-2 for coding Item J0100 — Pain Management:
“NON-MEDICATION PAIN INTERVENTION: Scheduled and implemented non-pharmacological interventions include, but are not limited to: biofeedback, application of heat/cold, massage, physical therapy, nerve block, stretching and strengthening exercises, chiropractic, electrical stimulation, radiotherapy, ultrasound and acupuncture. Herbal or alternative medicine products are not included in this category.”
Check Out New Example for Item K0710
CMS added a third example for Item K0710 — Percent Intake by Artificial Route, which now appears on pages K-16 and K-17:
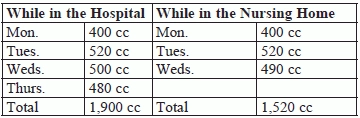
3. Mr. K has been able to take some fluids orally, however, due to his progressing multiple sclerosis, his dysphagia is not allowing him to remain hydrated enough. Therefore, he received the following fluid amounts over the last 7 days via supplemental tube feedings while in the hospital and after he was admitted to the nursing home.
Coding: K0710B1 would be coded 1,500 cc/day or less. K0710B2 would be coded 2,501 cc/day or more, and K0710B3 would be coded 1,500 cc/day or less.
Rationale: The total fluid intake within the last 7 days while Mr. K. was not a resident was 1,900 cc (400 cc + 520 cc + 500 cc + 480 cc = 1,900 cc). Average fluid intake while not a resident totaled 475 cc (1,900 cc divided by 4 days). 475 cc is less than 500 cc, therefore code 1, 500 cc/day or less is correct for K0710B1, While NOT a Resident.
The total fluid intake within the last 7 days while Mr. K. was a resident of the nursing home was 1,520 cc (510 cc + 520 cc + 490 cc = 1,520 cc). Average fluid intake while a resident totaled 507 cc (1,520 cc divided by 3 days). 507 cc is greater than 500 cc, therefore code 2, 501 cc/day or more is correct for K0710B2, While a Resident.
The total fluid intake during the entire 7 days (includes fluid intake while Mr. K. was in the hospital AND while Mr. K. was a resident of the nursing home) was 3,420 cc (1,900 cc + 1,520 cc). Average fluid intake during the entire 7 days was 489 cc (3,420 cc divided by 7 days). 489 cc is less than 500 cc, therefore code 1, 500 cc/day or less is correct for K0710B3, During Entire 7 Days.
Don’t Forget About ‘Unstageable’ Pressure Ulcers in M0610
CMS revised wording in #7 of Steps for Assessment under Item M0610 — Dimensions of Unhealed Stage 3 or 4 Pressure Ulcers or Unstageable Pressure Ulcer Due to Slough and/or Eschar (on page M-22):
“7. Considering only the largest Stage 3 or Stage 4 pressure ulcer or pressure ulcer that is unstageable due to slough or eschar, determine the deepest area and record the depth in centimeters…”
CMS Clarifies N0410 Coding for Certain Meds
Another revision appears in Example #1 for Item N0410 — Medications Received (page N-8):
“Coding: Medications in N0410 would be coded as follows: A. Antipsychotic = 3, resperidone is an antipsychotic medication, B. Antianxiety = 7, lorazepam is an antianxiety medication, and D. Hypnotic = 2, temazepam is a hypnotic medication….”