Learn From 5 Section G Tips To Advance Your ADL Coding
Don’t include these functional factors when coding items.
When it comes to coding Activities of Daily Living (ADLs) and other items in Section G — Functional Status, there are many hidden traps where you can make big mistakes. Follow these expert tips to avoid several common coding errors.
Tip #1: Paint an Accurate Overall Picture of Performance
When coding Item G0110 — Activities of Daily Living (ADL) Assistance, consider all episodes of the activity that occurred during the seven-day look-back period to achieve the most accurate coding of the resident’s self-performance, according to the Oklahoma State Department of Health (OSDH) Quality Improvement & Evaluation Service.
Important: Keep in mind that the resident’s performance may vary widely depending upon the time of day, medical condition, level of fatigue, staff assisting, and so on, OSDH said. Your responsibility is “to give the most accurate overall picture of the resident’s performance during the look-back period.”
Tip #2: Remember to Use the ‘Rule of 3’
Residents needing staff to push their wheelchairs isn’t uncommon, but coding this in Section G isn’t so simple. Like other ADLs, you need to use the “Rule of 3” to determine the proper coding (see page G-7 of the RAI manual for Rule of 3 instructions). OSDH provides the following example:
Scenario: Mr. B is an 80-year-old male who was admitted to the nursing home with a wound on his right foot due to stepping on a sharp object and then falling, causing a second wound on his left hand. While completing Mr. B’s quarterly assessment, you notice that the doctor ordered no weight bearing on Mr. B’s right leg until the wound on his foot healed.
Due to the wound on his left hand, Mr. B was also unable to self-propel his wheelchair, so staff members had to push him in his wheelchair multiple times and adjust the foot pedals so he could raise his legs and place his feet on them. During the last two days of the look-back period, you notice documentation in the medical record that the wounds on Mr. B’s right foot and left hand had healed and the doctor discontinued wound care.
The doctor ordered physical therapy to evaluate and treat Mr. B for strengthening and ambulation training with a walker. Therefore, for the seven-day look-back period, staff members pushed Mr. B in his wheelchair 25 times, but not every time.
How to code: For this scenario, you would code 3 — Extensive assistance. The resident is in the wheelchair, which now contains the resident’s weight, so the staff are providing weight-bearing assistance, the OSDH concluded.
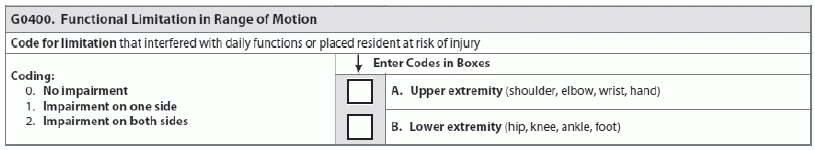
Tip #3: Know How to Code Lower Functional Limitation in ROM
How should you code Item G0400 — Functional Limitation in Range of Motion, and why is this item so important?
Functional limitation in range of motion (ROM) is a resident’s limited ability to move a joint that interferes with daily functioning, such as ADLs, or places the resident at risk of injury, according to the California Department of Public Health (CADPH) RAI/MDS office. For Item G0400, you must determine whether the functional limitation in ROM interferes with the resident’s ADLs or places the resident at risk for injury.
Tip: When completing Item G0400, “refer back to Item G0110 and view the limitation in ROM, taking into account activities that the resident is able to perform,” CADPH instructed. You can also find specific coding instructions on functional ROM limitations for upper and lower extremities on page G-36 of the RAI manual.
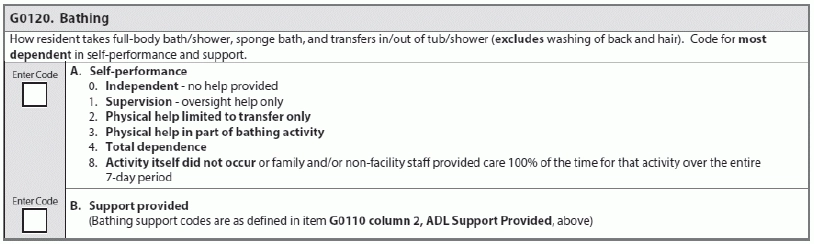
Tip #4: Define ‘Managing’ for Ostomy Coding
Coding management of an ostomy under toileting in Item G0110 (G0110I — Toilet use) can also be a little tricky, because many MDS coders become confused about whether this includes the staff “managing” the ostomy or just the resident.
What to do: First identify what the resident is able to do for herself, noting type and level of assistance that staff provided, if needed, OSDH stated. If the resident required oversight, encouragement or cueing three or more times in the seven-day look-back period, then code as 1 — Supervision in Column 1 (Self-Performance). For Column 2 (Support), determine if the resident required setup help only (1) or a one-person physical assist (2).
Tip #5: Understand What to Exclude from Coding
You have to consider a whole variety of factors when coding Section G, but some situations don’t fall into the coding categories even when you think they should. According to a recent presentation by Shirley Boltz, RN, RAI/Education Coordinator for the Kansas Department for Aging and Disability Services, here are a few items to keep in mind when completing Section G that are not included in the coding: