Consider Effect -- Not Intent -- For Physical Restraints
Know the definitions for different types of physical restraints.
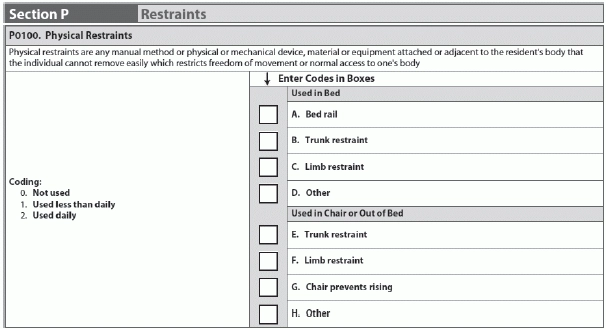
Although not prohibited for use in nursing homes, your MDS 3.0 coding of physical restraints can truly affect your quality measure outcomes. That’s why it’s vitally important to not only code Section P properly, but also institute practices in your facility to clarify the real meaning of physical restraint.
Definition: According to the MDS 3.0, a physical restraint is defined as: “any manual method or physical or mechanical device, material or equipment attached or adjacent to the resident’s body that the individual cannot remove easily, which restricts freedom of movement or normal access to one’s body.”
Why Intent to Restrain Doesn’t Matter
In P0100, you would code only the devices that have the effect of restraining the resident. “It’s not about the intent; it’s the effect upon the resident,” said Ann Spenard, MSN, RN, C, vice president of consulting services for Wethersfield, CT-based Qualidigm, in a recent Centers for Medicare & Medicaid Services (CMS) instructional session.
Example: You’re pushing Mr. Smith in his wheelchair when you need to stop for a few minutes to talk with another nurse. You lock Mr. Smith’s wheels so the wheelchair doesn’t roll around. Mr. Smith doesn’t have the agility in his legs or feet to unlock the wheels on his own.
Although you locked the wheelchair wheels mostly for safety reasons, because Mr. Smith cannot unlock the wheels on his own, this is a form of restraint — despite the fact that you didn’t intend to restrain him.
What ‘Removes Easily’ Really Means
“Removes easily” means that the resident can remove the item or device intentionally “in the same manner that it was applied by the staff,” Spenard explained. “So it’s not going to be considered a restraint if the resident can take it off.”
Example: You place a foam “lap buddy” in the front of Mrs. Brown’s wheelchair. Mrs. Brown can remove the lap buddy on her own, but only after she fiddles with it for a long time. Sometimes, Mrs. Brown takes up to an hour or more to remove the lap buddy. Mrs. Brown cannot remove the lap buddy “easily,” so this is considered a form of restraint.
Advice: If you ask a resident to remove something, she should be able to do so easily and on-command, Spenard said. Put a system or process in place to make sure a device or item “doesn’t transition from something that does not meet the criteria for a restraint to something that does meet the criteria.”
Consider the Resident’s ‘Freedom of Movement’
The definition of physical restraint also refers to “freedom of movement,” which the MDS defines as: “any change in place or position for the body, or any part of the body that the person is physically able to control or access.” The resident must have freedom of movement in order for the method, device, material or equipment to not be considered a physical restraint.
Example: Mr. Jones wants to scratch his knee, but a tray is preventing him from reaching his knee. He cannot swivel the tray on his own. This is preventing Mr. Jones’ freedom of movement and freedom of access to his body. This has the effect of a restraint on the resident.
So when you’re coding Section P in the MDS, you need to not only talk with staff across all shifts and look at the medical record, but also “observe the resident to determine the effect of the resident’s normal function,” Spenard stated. “And do not focus on the type or the intent or the reason for the use. It’s the effect upon the resident.”
Don’t Look at Restraints as Cookie-Cutter
“This section, along with other sections in the MDS, is not black and white,” Spenard cautioned. “It’s gray and various shades of gray.”
Meaning: “So, one device may be a restraint for me and may not be a restraint for someone else,” Spenard explained. No item, device or practice is “always” or “never” a physical restraint. “You have to look at the particular resident,” she noted.
Know Your Physical Restraint Definitions
According to QSource (www.qsource.org), part of the CMS Quality Improvement Organizations, the following are common MDS 3.0 Section P definitions that you should know: