Prevent Your ADL Coding From Sinking Your MDS-Focused Survey
Beware of 5 mistakes staff could be making when coding ADL tasks for their shift.
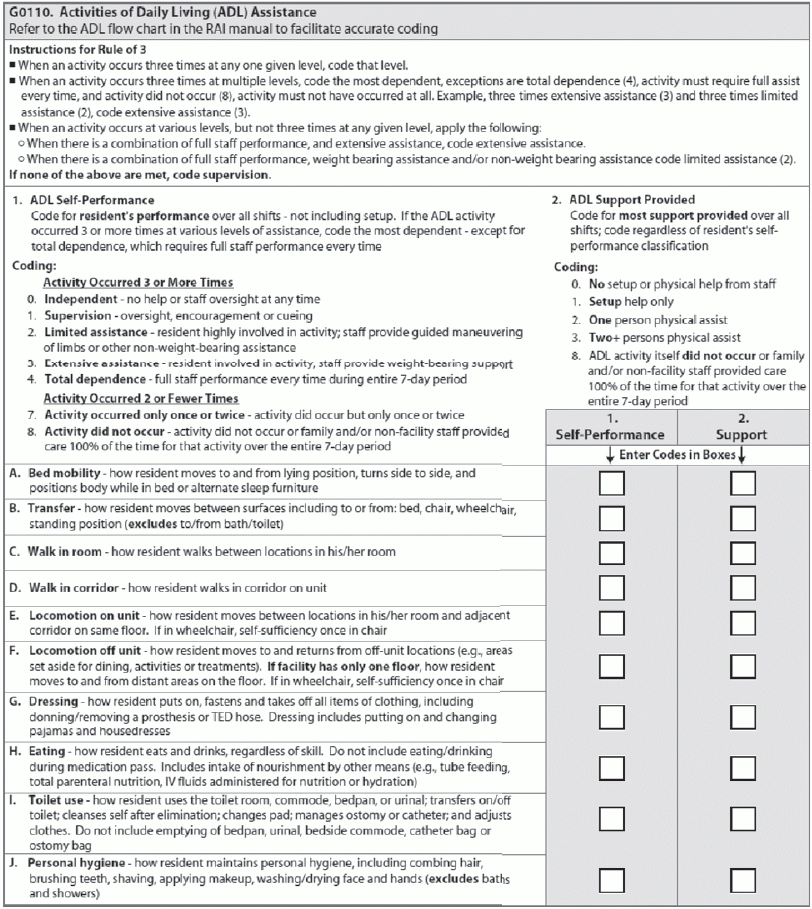
Now that the MDS Focused Surveys are in full swing, you must prepare for scrutiny of key problem areas in your MDS 3.0 coding and assessments. And one area that’s come under surveyors’ microscope is coding Item G0110 — Activities of Daily Living (ADL) Assistance.
Surveyors are looking at late loss ADLs, due to HHS Office of Inspector General (OIG) findings that many show disagreement between the MDS record and the medical chart. During the 2014 MDS Focused Survey pilot, which the Centers for Medicare & Medicaid Services (CMS) conducted in five states (Illinois, Maryland, Minnesota, Pennsylvania, and Virginia), late loss ADLs accounted for 15.4 percent of the deficient areas cited.
Cost: Also, ADLs impact approximately 30 percent of nursing facility revenue, according to a Jan. 21 training by Terry Raser, RN, RAC-CT, C-NE, CIC, senior consultant with LW Consulting Inc., for the Pennsylvania Association of Nurse Assessment Coordinators. ADLs also directly affect your facility’s quality measures and Five Star rating.
Don’t Restrict Training to Only the MDS Coordinator
But unfortunately, miscoding in Section G’s ADLs is common, warned Becky LaBarge, RN, RAC-CT, RAC-MT of RLL Consulting in a recent presentation to the Kansas Health Care Association/Kansas Center for Assisted Living. That’s why LaBarge emphasized the importance of training on ADL coding for these key staff members:
And there are two ways to educate staff on ADL coding, Raser noted. One way specifically addresses coding for the staff member’s eight-hour shift, and the other way covers coding on the MDS from the daily ADL trackers.
Educate to Avoid 5 Common Coding Mistakes
Best strategy: When you’re educating staff on coding for their shift, “it is extremely important to teach staff the definition of each task that affects that ADL,” Raser stressed. Here are some common coding mistakes in understanding the ADL tasks in Item G0110:
1. Resident doesn’t sleep in the bed: If a resident doesn’t sleep in a bed but maybe in a recliner chair, make sure staff are not coding 8 — Activity did not occur in G0110A — Bed mobility. Instead, educate staff to code G0110A according to how the resident is positioned in the recliner.
2. Transfer to bath or toilet: Note that G0110B — Transfer does not include bath or toilet, because you code this elsewhere in the MDS. Make sure your staff understand this.
3. Resident doesn’t come out of room: Do staff understand that Item G0110E — Locomotion on unit includes locomotion in the room as well as on the unit? If staff are coding 3 — Extensive assistance for Item G0110C — Walk in room, but then code 8 — Activity did not occur in G0110E, this could be a discrepancy in coding and a red flag to surveyors.
4. Who fed the resident: Investigate who is feeding the resident if he is not able to feed himself without assistance. Make sure a staff member is not coding 8 — Activity did not occur in G0110H — Eating just because that staffer didn’t feed the resident that day and someone else did or because the nurse takes care of the feeding tube.
5. Resident didn’t use the toilet: Likewise, investigate further if staff are coding 8 — Activity did not occur for G0110I — Toilet use just because the resident didn’t use the toilet. Did the resident use a bed pan or was the resident just incontinent on the pad? The coding for Item G0110I needs to reflect these scenarios. Also, don’t include emptying bedpans, urinals, bedside commodes, catheter bags, or ostomy bags.
Locate & Verify the Data
Gathering together all the data, notes, and worksheets from other staff members to put together an ADL coding scenario can be daunting. And this job becomes even more difficult when you can’t locate all the data or when you don’t know where your data comes from.
Here’s what you can do to make your job easier — and ensure that your ADL coding is accurate. According to LaBarge, you must pay close attention to how you and other staff collect data for coding ADLs, including how you:
When You Need an ADL Clarification Note
Finally, you should include an ADL clarification note if the “ADL coding does not look like the resident,” Raser said. For instance, the resident always requires two-person assist but this is not coded in the MDS. The ADL clarification note should identify the task, the accurate self-performance type, and the number of times the task occurred during the seven-day look-back period, as well as the date of the note and the signature and title of the person writing the note.
Important: “Make sure you are going back to staff and questioning them about the coding on the ADL tracker if it doesn’t look like the resident or the coding doesn’t make sense,” Raser instructed. “For those facilities that have software where you push a button to pull the ADL information to the MDS, please make sure you are reviewing the daily ADL tracker sheet to see if the coding is accurate and there aren’t inappropriate codes that could give you the wrong overall code.”