Support Your Modifier 66 Use With Proof of Team Surgery Necessity

Recognize that surgeons of the same specialty do not constitute a team.
Every time your surgeon performs a procedure with at least two other surgeons, you should consider that a team surgery, right? Not so fast.
Having involvement from multiple physicians or other qualified health care professionals is not the only way to define a surgical team. If you’re stymied by this, continue on to read about modifier 66 (Surgical team) and eliminate the confusion.
Show Proof of the Need for a Surgical Team
A surgical team is typically three or more providers of different specialties and other highly skilled clinicians performing work on the same procedure, often using complex surgical equipment.
“Under some circumstances, highly complex procedures (requiring the concomitant services of several physicians or other qualified health care professionals, often of different specialties, plus other highly skilled, specially trained personnel, various types of complex equipment) are carried out under the ‘surgical team’ concept,” explains John F. Bishop, PA, CPC, CPMA, CGSC, CPRC, director surgical coding and auditing services, senior multispecialty coder, auditor and educator at The Coding Network, LLC in Tampa, Fla. “Such circumstances may be identified by each participating individual with the addition of modifier 66 to the basic procedure number used for reporting services.”
The record must show medical necessity for having a team of surgeons working together because team surgeries are paid for on a “by-report” basis.
Example: A team surgery might be appropriately billed with modifier 66 for surgeons performing an organ transplant. For example, procedures such as a liver transplant (47135-47136, Liver allotransplantation ... or an intestinal transplant (44135-44136, Intestinal allotransplantation ...). The team could consist of a general surgeon specializing in organ transplant, a gastrointestinal surgeon, a vascular surgeon, neurosurgeon, and maybe a plastic surgeon to perform all the various portions of these procedures.
Pointer: There may be procedures performed during the case that can be separately billed by the performing surgeons.
Your physician(s) must provide details in his documentation describing the procedure performed and stating that he was a part of a team. Each provider reports the same procedure code with modifier 66 attached. This tells the payer that the amount for the procedure should be divvied up between a team of providers instead of paid to just one. The documentation of all of the providers involved is necessary to determine if team surgery can be billed or if some services should be billed by one person, some billed as an assistant, or some billed as the team approach.
Counting the Number of Surgeons is Not All You Need to Know
There could be a situation when there are three or more surgeons involved in a procedure but it is not considered a “surgical team.” There could be co-surgeons and an assistant surgeon, all of the same specialty, working on the same procedure. You would report the appropriate procedure code but you would not attach modifier 66. Instead you might use modifier 62 (Two surgeons) or modifiers 80 (Assistant surgeon), 81 (Minimum assistant surgeon), or 82 (Assistant Surgeon [when qualified resident surgeon not available]), depending on the clinical situation.
How it works: If two surgeons of different specialties perform a procedure in the same session or they perform the parts of the procedure simultaneously, attach modifier 62 to the procedure code. If surgeons of different specialties are each performing a different procedure, with different procedure codes, you don’t need a modifier.
Example: Your gastroenterologist decides to place a percutaneous endoscopic gastrostomy (PEG) tube (43246, Esophagogastroduodenoscopy, flexible, transoral; with directed placement of percutaneous gastrostomy tube) for a patient suffering from dysphagia that has caused weight loss over the past six months. Under sedation, your gastroenterologist uses a flexible endoscope to perform an upper gastrointestinal duodenoscopy to determine the site where the gastrostomy tube can be inserted.
Another gastroenterologist places the gastrostomy tube through an incision made in the abdominal wall using the reference of the location determined by the endoscopic procedure. The gastrostomy tube is held in place by a retention disk placed along the anterior abdominal wall.
Since the work performed by both the gastroenterologists is part of the same procedure, you will use the same procedural code for reporting both services, but you would not use modifier 66. Instead, you need to use modifier 62 to both the claims in order to help the payer identify that there were two gastroenterologists involved in performing the same procedure on the patient.
Bottom line: A surgical team would have to consist of three surgeons from different specialties working under the same anesthesia in order for you to use modifier 66. This would be a very rare situation such as an organ transplant as noted in the example above. Most procedures that consist of teams have two surgeons and an assisting that you would most likely report using other modifiers.
Stay tuned for an article in a future issue of Modifier Coding Alert on modifiers 80, 81, and 82.
Jump to the Fee Schedule For More Help With Surgical Teams
If you feel like you’re guessing on when you can attach modifier 66 to a surgical procedure, take a quick look at the fee schedule for a definitive answer.
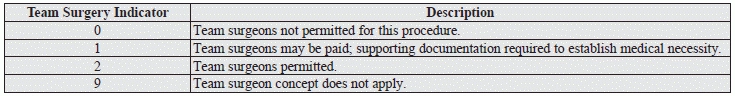
If you see a “0” or “9” in the” TEAM SURG” column, you should never apply modifier 66 to that code. The zero indicates that team surgeons are not permitted for the procedure, and the nine indicator means the concept does not apply. Medicare will never allow billing for a surgical team with any procedure that includes a “0” or “9” indicator in the fee schedule’s “TEAM SURG” column.
If you find a “1” in the” TEAM SURG” column, Medicare may allow modifier 66 with supporting documentation that establishes medical necessity for the surgical team.
If you find a “2” in the “TEAM SURG” column, Medicare will permit modifier 66 with that code.