You Be the Coder:
Dust Off Modifier 78 for Return Trip to Surgery
Published on Wed Aug 20, 2014
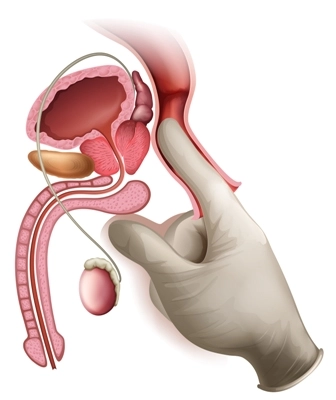
Question: One of our physicians has a patient that had an incisional biopsy of the prostate in the op surgery department (post-op period of 10 days). Path findings were positive for cancer. He was admitted for radical prostatectomy within the global surgical period. Should I attach modifier 78 to the radical prostatectomy?
Oregon Subscriber
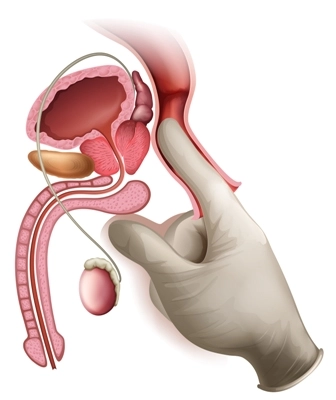
Answer: Yes, since your surgeon performed the procedure within the global period of the biopsy, you should use modifier 78 (Unplanned return to the operating/procedure room by the same physician or other qualified health care professional following initial procedure for a related procedure during the postoperative period).
In a situation when your surgeon performs another procedure that has no correlation with the initial procedure that was performed, you should not use the modifier 78. Instead, you should attach modifier 79 (Unrelated procedure or service by the same physician or other qualified health care professional during the postoperative period) to the CPT® code of the second procedure.
Note: While your physician doesn’t have to take the patient back to the operating room for you to use modifier 79, a return to the OR is required for modifier 78 use