Use G Modifiers to Stay 'Mainstream'
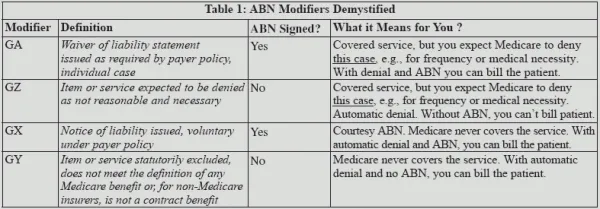
Confused about ABN-related modifiers? Check out this table.
When the physician performs a service that Medicare might not cover, you should ask these questions:
1. Do we have a signed advance beneficiary notice (ABN) on file, if necessary?
Reason: Whenever your practice provides a service that Medicare might not cover, or not cover completely, the ABN notifies the patient of that fact. Having a signed ABN will allow you to bill the patient for the service. When your practice provides any services that Medicare might not pay for, it’s also up to you to select the proper modifier for the encounter.
Many practices shun these modifiers for various reasons. Those practices should reconsider their stances on ABN modifiers, warns Leslie Johnson, CPC, CSFAC, chief coding officer at PRN Advisors in Palm Coast, Fla. Johnson recommends using the modifiers whenever Medicare requires, or it could identify the practice as an outlier.
“Rules are rules. CMS is tracking every single code, and that includes the modifiers. Codes that are reported — or not reported — are indicative of patterns that are tracked by the data-mining systems,” Johnson explains.
Bottom line: Deviate from the norm one way or another, and payers could take notice, Johnson warns.
Use this: Check out this table aimed at making it easier to file clean claims for potentially uncovered Medicare services.
2. Did I append the proper modifier based on the encounter notes?