Know Vertebroplasty/Kyphoplasty Differences for Correct Coding
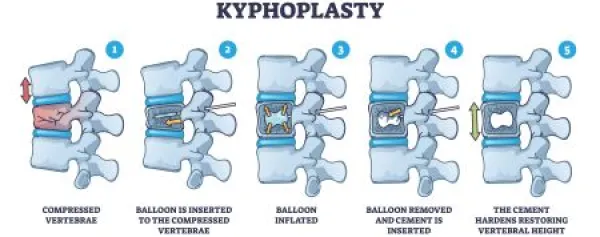
Affected bone being elevated? That’s a kyphoplasty. Kyphoplasty and vertebroplasty are minimally invasive procedures used to treat painful spinal fractures. Both procedures involve injecting a specialized bone cement into the fractured vertebra to stabilize it and relieve pain. Purpose: These procedures are typically used to treat traumatic spinal fractures, osteoporosis-related compression fractures, and fractures caused by bone tumors on the vertebrae. Read on for information on the diagnostic and treatment options available when a patient needs a vertebroplasty or kyphoplasty. E/M Will Precede Any Vertebroplasty/Kyphoplasty The initial encounter, where patients will present to their provider with their complaints, should be billed using the appropriate evaluation and management (E/M) codes based on setting: The physician will perform a physical exam to review the patient’s symptoms and review the results of several tests, which may include: Know Differences to Choose Correct CPT® Code The critical distinction between a vertebroplasty and a kyphoplasty is which CPT® codes you’ll choose for each surgery. Here are the codes you’ll choose from for a vertebroplasty: These three codes cover a percutaneous vertebroplasty, which involves injecting bone cement into the vertebral body. Add-on code +22512 can be used with either of the above parent codes and should be billed per additional vertebral body. For example, if the surgeon performs a vertebroplasty of C3-C7, you’ll report 22510 and +22512 x 4. If notes indicate the surgeon performed kyphoplasty, your coding options change to the following: Similar to the vertebroplasty codes, add-on code +22515 would apply to additional levels of the thoracic or lumbar regions when coding 22513 or 22514. What differentiates these two procedures is the vertebral body augmentation performed during kyphoplasty. Vertebroplasties involve a simple cement injection into the fractured vertebrae. While kyphoplasty includes this step, it also involves elevating the affected bone with a mechanical device before injecting cement. Be Aware of the Verbiage “Vertebroplasties” performed during a spinal fusion can often be confusing. These are often documented as a vertebroplasty in the operative report but are integral to the fusion procedure. Consider this note: “We placed a fenestrated screw at T11 and injected vertebroplasty under live fluoroscopy.” Note the injection of cement was documented as part of a large fusion procedure. While some might see this and capture 22513 for a vertebroplasty, that would be incorrect. Placing cement into a vertebra solely for the purpose of holding screws in place during a spinal fusion cannot be considered a true vertebroplasty and should not be separately captured as such. Include This Procedural Documentation in Claim Notes For vertebroplasty, documentation should indicate no attempt was made to restore vertebral height or create a cavity for the cement. If the surgeon creates a cavity, the kyphoplasty codes would apply. Operative reports should clearly describe the fracture location, the number of levels treated, the maneuvers and devices used to inject cement into the vertebral body via a percutaneous approach, and the cement volume. The provider should also note whether they injected the cement into the vertebral body unilaterally or bilaterally. Venography performed during the operative session is included and should not be billed separately. The surgeon might also perform a bone biopsy at this time for diagnostic purposes, but you should not report it separately. In kyphoplasty, the provider will use a balloon and needle, inserted into the affected vertebrae and inflated to restore the height of a collapsed or crushed vertebra. After that, the surgeon injects bone cement into the vertebral space to prevent future fractures. The injection may be performed on one or both sides of the vertebra. Similar to the vertebroplasty, a diagnostic bone biopsy would also be included in a kyphoplasty. Check Out This Clinical Example A patient presents to the ED with severe back pain. Upon arrival, the attending physician orders imaging to evaluate the location and severity of the pain. The patient is found to have T4-T7 compression fractures, based on the extensive osteoporosis diagnosed previously in the patient’s records and verbally confirmed by the patient. The attending physician then sends the patient for kyphoplasty, which the neurosurgeon performs. This encounter should be reported as 22513 for the T4 fracture repair and +22515 x 3 for additional thoracic fracture fixes. Be sure to append M80.08XA (Age-related osteoporosis with current pathological fracture, vertebra(e), initial encounter for fracture) to 22513 and +22515 x 3 to represent the pathological fracture due to osteoporosis. Final Thoughts The distinction in choosing the correct code for vertebroplasty and kyphoplasty lies in the operative report. The medical record that orders the procedure should detail the intent, but you should always rely on the surgical report for validation. The principal factor is whether the vertebral body is being augmented with a cavity before cement is placed. When in doubt, query your provider before applying a code. Jessica Sullivan, CPC, COBGC, COSC, Consultant,
Pinnacle Enterprise Consulting Services (PERCS)

