Reach Separate Service Threshold on E/Ms With Minor Procedures
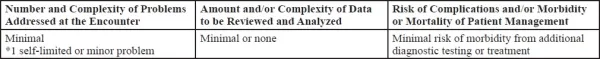
New year, new rules, new way to I.D. separate E/Ms with surgeries. Some coders might be having a tougher time this year identifying separate office/outpatient evaluation and management (E/M) services that occur with minor procedures. Why? In case you haven’t heard, the office/outpatient E/M coding experience is completely different this year. How you choose an E/M code — and how an encounter can qualify for each E/M level — has changed. As a result of this change, you’ll need to adjust your coding on potential procedure- E/M combo claims for 2021 as well. In fact, one of the only things that hasn’t changed is that you’ll append modifier 25 (Significant, separately identifiable evaluation and management service by the same physician or other qualified health care professional on the same day of the procedure or other service) to all separate E/ Ms that occur in conjunction with a minor surgery. Help’s here: Before you report another minor procedure with a separate E/M, check out this advice from Lori A. Cox, MBA, CPC, CPMA, CPC-I, CEMC, CGSC, CHONC, on how to navigate the procedure-E/M conundrum in 2021. Straightforward MDM Marks 99202, 99212 The driver in the E/M changes is how you’ll decide between E/M levels: total encounter time or medical decision making (MDM) are the only criteria by which to choose an E/M code now — and you need to pick one or the other. So you need to make sure you’re lining up your potential separate E/Ms with time or MDM, not the “three key components” of previous years’ E/M coding options (history, examination, MDM). This could be trickier than you think, as Cox illuminated during her recent presentation at HEATLHCON 2020 Regional Virtual Conference: “E/M Guidelines 2021 — Office Visits With Minor Procedures.” (CPT® made changes to all office/outpatient E/M code descriptors for 2021, but for the purposes of this article we are only listing a pair of the new descriptors. For a full rundown of new descriptors, check your CPT® 2021 manual.) Cox reminded coders to reach the straightforward medical decision making (MDM) or the time components in the code descriptors in order to report: In order to achieve straightforward MDM during an E/M service, the visit must meet two of these requirements: Report separate E/M: According to Cox, here are two instances when you might be able to report a separate 99212-25 along with a procedure code: Do not report separate E/M: According to Cox, here are two instances when you cannot report a separate 99212-25 along with a procedure code: