Hand In Claims With Finger/Toe Modifiers, When Required
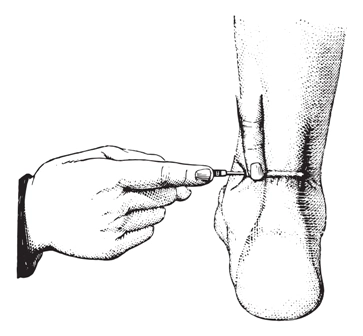
If you sleep on these modifiers, it could end up costing you. In general, orthopedic practices perform procedures on patients’ fingers and toes more than other specialties. Therefore, these practices need to be experts when considering whether or not to use finger/toe modifiers to indicate the location of treatments. Bottom line: Medicare’s rule is that you should use finger/toe modifiers whenever they are necessary to paint the most accurate picture of the patient’s injuries and how they correlate to the provider’s services. Many private payers follow Medicare’s lead on policy, so it’s likely that many of those payers also require the modifiers. Follow this expert advice on finger/toe modifiers. Understand Purpose of Modifiers When your physician performs services on a patient’s fingers or toes, you might need to use modifiers FA (Left hand, thumb) through F9 (Right hand, fifth digit) for fingers or TA (Left foot, great toe) through T9 (Right foot, fifth digit) for toes, says Mary Falbo, MBA, CPC, CEO of Millennium Healthcare Consulting, Inc. in Lansdale, Pennsylvania. Logic: These F/T modifiers serve a serious purpose: improving patient care. “They prevent erroneous denials when duplicate CPT®/HCPCS codes are billed to report separate procedures on different anatomical sites, or different sides of the body,” Falbo says of F/T modifiers. “For example, physician performs a procedure on more than one toe and/or finger at the same operative session. “Also, reporting these modifiers will potentially avoid medical necessity denials in the future, since you are indicating that this is a different finger/toe,” Falbo continues. Medicare recognizes these modifiers, so most Medicare payers would be familiar with them. As usual, you should check with your private payers for their individual stances on F/T modifiers. According to experts, you should take the time to check each payers’ policy on the F/T modifiers. Policies can vary widely depending on insurer or procedure, says Peggy Bryant, CPC, CPMA, provider coding compliance coordinator for Dickinson County Healthcare System in Iron Mountain, Michigan.