Understand the Complexities of Shoulder Arthroplasty Coding
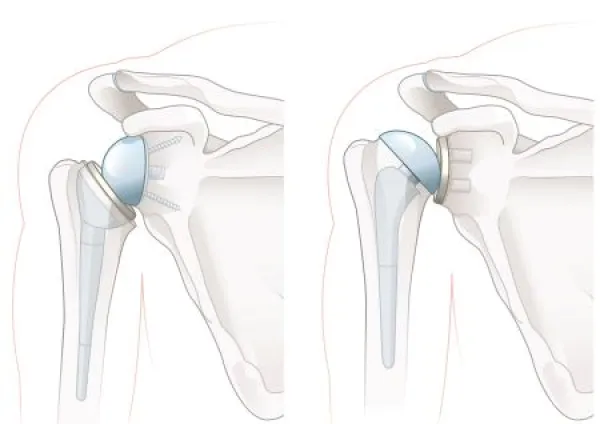
Know when to report arthroplasty revisions. Patients experiencing pain and stiffness in their shoulders might require surgery to repair or replace the joint to ensure continued functionality. Orthopedic surgeons have multiple options for shoulder arthroplasty, and as an orthopedic coder, you need to know how to report the procedures and associated diagnoses to help ensure the practice receives reimbursement. Familiarize yourself with shoulder surgeries and the conditions that warrant the procedure. Get to Know the Types of Shoulder Arthroplasty Arthroplasty is a surgical procedure where the surgeon removes damaged portions of bone and replaces structures with implants. A patient can experience stiffness, weakness, and pain in the shoulder joint when the ball-and-socket joint is damaged. Joint explanation: The shoulder is an example of a ball-and-socket joint, where the upper arm bone’s round head (ball) fits into the shoulder’s socket. Surgeons perform partial or total shoulder arthroplasties to treat the patient’s condition. During partial shoulder arthroplasty, the surgeon replaces just the ball of the joint with an implant. The physician performs this procedure when the rounded head of the upper arm is damaged, but the shoulder socket is intact. You’ll assign 23470 (Arthroplasty, glenohumeral joint; hemiarthroplasty) to report a partial shoulder replacement surgery. Hemiarthroplasty is a term that means partial replacement; so, if you see this term or partial shoulder arthroplasty in the procedure report, you’ll know to report 23470. Total shoulder arthroplasty involves the physician removing and replacing both the ball and socket of the joint. A reverse total shoulder replacement is the same as a total shoulder replacement, but the implants are switched. The provider attaches the ball to the shoulder blade and attaches the socket to the upper arm. Report 23472 (… total shoulder (glenoid and proximal humeral replacement (eg, total shoulder))) when the surgeon performs a total shoulder arthroplasty. This includes removal and replacement of the damaged upper humerus bone and shoulder socket. You’ll assign this code regardless of whether the provider performs a traditional total shoulder joint replacement or a reverse total shoulder arthroplasty. Report Arthroplasty Revisions Correctly Over time, the implants may become dislodged or break, which will require a surgeon to remove and replace the pieces to ensure joint mobility. The surgeon may use tissue from another part of the body, called an allograft, to stabilize the new prosthesis. Assign 23473 (Revision of total shoulder arthroplasty, including allograft when performed; humeral or glenoid component) when the provider performs a shoulder arthroplasty revision that affects either the humeral (upper arm) or glenoid (shoulder socket) component. On the other hand, if the physician revises both components of the total shoulder arthroplasty, then you’ll assign 23474 (… humeral and glenoid component) for the procedure. Identify Shoulder Injury ICD-10-CM Codes Orthopedic surgeons perform shoulder arthroplasty to alleviate pain, stiffness, and other symptoms the patient is experiencing due to the damaged joint. You must show medical necessity for the shoulder surgery to ensure reimbursement; otherwise, the payer will deny your claim. You’ll exhibit the reason for the procedure through detailed documentation and assigning the correct ICD-10-CM codes. Common conditions that cause joint damage include: Remember: According to the ICD-10-CM Official Guidelines, if a fracture isn’t documented as displaced or not displaced, you’ll report the fracture as displaced. Mike Shaughnessy, BA, CPC, Development Editor, AAPC