Get Easy Answers to 3 Top Laryngeal Procedure Questions
Like it or not, ‘unlisted’ sometimes is the best choice.
Your otolaryngologist can perform a wide range of laryngeal procedures, from in-office injections to treat various conditions to lesion removal and cancer surgery. Read on for your coding answers to three common scenarios.
Turn to ‘Unlisted’ for Flexible Guidance With Injection
Question 1: Our physician used flexible endoscopic guidance before administering percutaneous laryngeal injections. How should we code for this?
Answer 1: CPT® does not include a code specifically for percutaneous laryngeal injections when the surgeon uses flexible laryngoscopy for guidance and needle placement. As a result, your best option is to report the “unlisted” laryngeal code, 31599 (Unlisted procedure, larynx).
Remember that in this situation, code 31599 includes both the injection and the flexible laryngoscopy. However, you might be able to also submit a HCPCS J code for the material your physician injects, such as J0585 (Injection, onabotulinumtoxina, 1 unit) that the otolaryngologist injects into the larynx to treat spasms.
Rigid scope change: You’ll code the encounter differently if the otolaryngologist administers the injections while using a rigid scope for direct laryngoscopy. In that case you’ll choose between 31570 (Laryngoscopy, direct, with injection into vocal cord[s], therapeutic) and 31571 (… with operating microscope or telescope). Make sure you include the “J” code for the drug that is injected.
Report 31599 for Injection Through Flexible Scope
Question 2: What code do we report if the physician administers the laryngeal injection through the flexible scope?
Answer 2: Physicians sometimes perform injections through the operating port of a flexible fiberoptic or flexible distal-chip laryngoscope. Once again, the current edition of CPT® does not include a code for this specific service. You should file the claim with 31599.
Codes 31570 and 31571 are not correct for injections performed using either flexible fiberoptic or flexible distal-chip endoscopic guidance. You can use 31570 or 31571 when setting your fee and reference these codes when communicating to the third party insurance company as a reference point that demonstrates an equivalent service in determining the value and fee for the unlisted code.
Code 31580 Covers Both Keel Insertion and Removal
Question 3: Our otolaryngologist performed a keel removal that I believe qualifies for 31580 (Laryngoplasty; for laryngeal web, 2-stage, with keel insertion and removal). I’ve seen information before stating that, “During a separate operative session after the larynx has had time to heal, the physician reenters the operative site through the same incision and removes the keel.” The physician removed the keel under general anesthesia. I know we cannot bill 31580 a second time, but can we report anything?
Answer 3: According to coding guidelines, 31580 includes the insertion and the removal of the keel. That means you should not report a separate code for the keel removal.
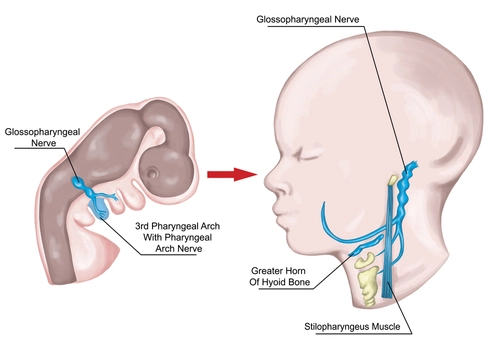
During the procedure, the surgeon often performs a tracheostomy to access the patient’s larynx and the laryngeal web around the vocal cords (though he or she might use another mode to reach the larynx). The surgeon removes the web tissue and inserts a keel, which is an artificial piece that creates some space between the vocal cords. After the larynx heals, the surgeon performs a second procedure to remove the keel. He accesses the larynx through the original laryngotomy incision.
You should report 31580 for the original procedure but nothing for the follow-up keel removal. The code has an RVU value of 34.97, which is substantial and should cover both services.