Clip the Correct Modifier for Reporting Incomplete Colonoscopy
Plus: Don’t miss how reimbursement can change in 2016.
In last month’s issue of Outpatient Facility Coding Alert, we studied some important aspects of colonoscopy code selection, including selecting an ICD-10 diagnosis and knowing whether to report CPT® or HCPCS procedure codes. Now it’s time to brush up on another important factor related to these procedures: being confident when reporting an incomplete colonoscopy.
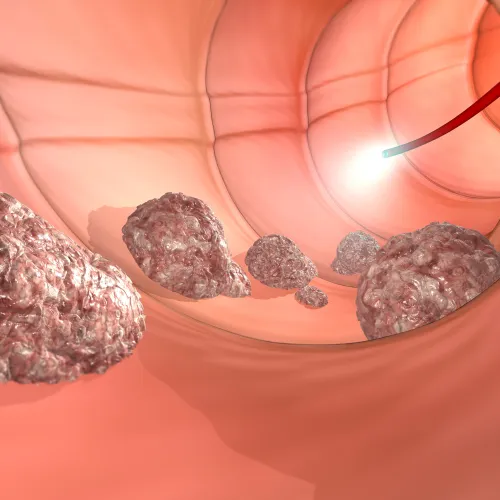
Starting point: It isn’t uncommon for a surgeon to plan a screening or diagnostic colonoscopy but, due to unforeseen circumstances, be unable to complete the procedure.
Prior to calendar year (CY) 2015, when reporting services to Medicare, if the provider advanced the scope past the splenic flexure, you would consider a screening colonoscopy to be “complete,” and report the appropriate screening code: G0105 (Colorectal cancer screening; colonoscopy on individual at high risk) or G0121 (Colorectal cancer screening; colonoscopy on individual not meeting criteria for high risk), depending on the patient’s risk factors, with no modifier appended. Medicare would pay the standard reimbursement rate for the coded procedure. But, if the physician prepped the patient for a screening colonoscopy and did not advance the scope past the splenic flexure due to obstruction, patient discomfort, or other complications, you would append modifiers, as appropriate.
Beginning in CY 2015, the CPT® instruction changed the definition of an incomplete colonoscopy to a colonoscopy that does not evaluate the entire colon. In accordance with this change, the Centers for Medicare and Medicaid Services (CMS) applied specified values in the Medicare Physician Fee Schedule (MPFS) database for the following codes:
For more information, refer to: https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNMattersArticles/downloads/MM9317.pdf.
Medicare Looks for Modifier 53 for Professional Billing
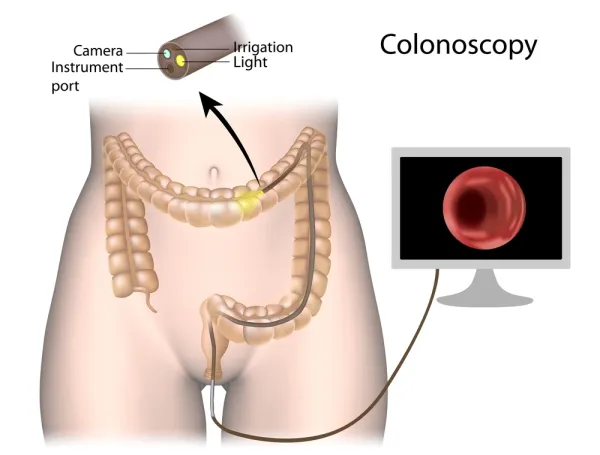
When a screening colonoscopy shifts to a diagnostic, you move from HCPCS to CPT® codes (such as 45378, Colonoscopy, flexible; diagnostic, including collection of specimen(s) by brushing or washing, when performed [separate procedure]). If the diagnostic procedure is stopped before its completion, Medicare and other payers that follow Medicare guidelines direct you to append modifier 53 (Discontinued procedure) to 45378.
“Note that in the facility setting you would report modifier -73 or -74, as appropriate.” cautions Sarah L. Goodman, MBA, CHCAF, COC, CCP, FCS, President, CEO, and principal consultant for SLG, Inc, in Raleigh, N.C
Information: You can find these instructions in Chapter 12, Section 30.1.B of the Medicare Claims Processing Manual. Medicare also includes a separate fee schedule line item for 45378-53, consistent with the MCPM guidelines, which states: “An incomplete colonoscopy (e.g., the inability to extend beyond the splenic flexure) is billed and paid using colonoscopy code 45378 with modifier 53. Although, failure to extend/evaluate beyond the splenic flexure could also mean that a sigmoidoscopy 45330 (rather than a colonoscopy, 45378) has been performed. However, 45330 will not be reported in this scenario since the physician aimed to perform colonoscopy (which remained incomplete due to inability to extend the scope beyond splenic flexure).”
AMA Gave Different Directions but Now Aligned with CMS
Previously, CPT® advised that a colonoscopy code should be reported with modifier 52 [Reduced services] when incomplete. However, the 2015 CPT® Manual states: “When performing a diagnostic or screening endoscopic procedure on a patient who is scheduled and prepared for a total colonoscopy, if the physician is unable to advance the colonoscope to the cecum or colon-small intestine anastomosis due to unforeseen circumstances, report 45378 (colonoscopy) or 44388 (colonoscopy through stoma) with modifier 53 and provide appropriate documentation.”
Important note: The above guideline assumes that the physician intended to perform a colonoscopy rather than a sigmoidoscopy. If the physician intended to perform a sigmoidoscopy, you would report 45330 (Sigmoidoscopy, flexible; diagnostic, including collection of specimen[s] by brushing or washing, when performed [separate procedure]) rather than 45378.
Watch for Revised Payments in 2016
As mentioned above, the 2015 CPT® manual redefined an incomplete colonoscopy as a “colonoscopy that does not evaluate the entire colon,” according to the American Gastroenterological Association.
As a result, CMS is updating payments for incomplete colonoscopies. Here are three things to know when filing these claims: