How Do You Code For a Probable Lung Abscess?
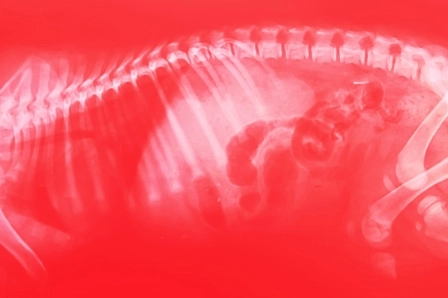
Question: The provider refers a patient, otherwise afebrile, with a vague chest pain for X-ray. The X-ray shows a lung mass, and the provider documents “Lung mass, probable abscess.” How do we code for this situation?
Texas Subscriber
Answer: ICD-10-CM guidelines require you to the highest level of specificity. It is inappropriate to code diagnoses documented as “probable”, “suspected”, “questionable”, “rule-out”, or differential diagnosis. Instead, report the ICD-10 code for the condition with the highest degree of certainty. This would include signs, symptoms, abnormal test results, etc.
In this case, you may assign code R22.2 (Localized swelling, mass and lump, trunk) for the mass in chest. If the provider had documented “lung mass due to lung abscess,” then you could assign code J85.2 (Abscess of lung without pneumonia).




