You Be the Coder:
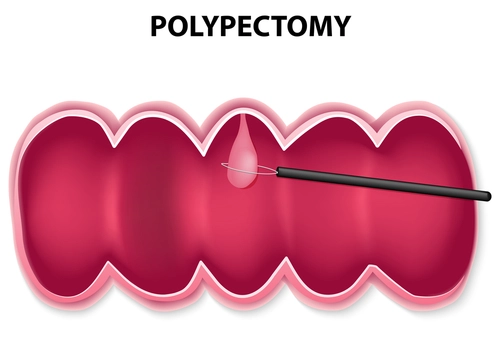
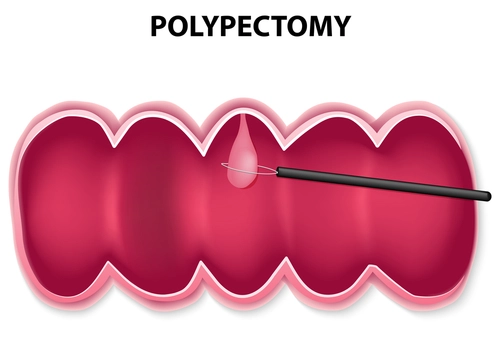
How to Time Your Polypectomy Coding
Published on Tue Aug 26, 2014
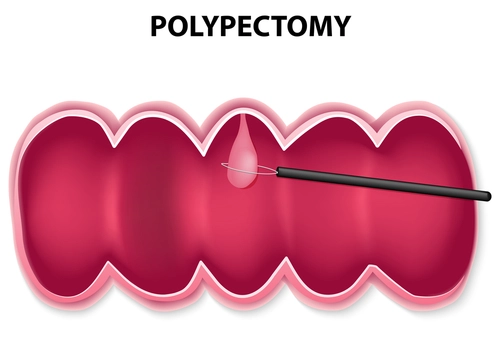
Question: Do we need to wait for the final pathology report before coding a polypectomy?
Texas Subscriber
Answer: Physicians wait for the final pathology report to see if the polyp is benign or malignant before determining the need for other treatment and the proper interval for the next surveillance colonoscopy, and the same holds true for coders. Whether or not you’re dealing with a full-blown colorectal cancer, you should look at the different terms used to describe benign or malignant colonic polyps to help with your code selection. Some of these include:
Adenomas including tubular adenomas and tubulovillous adenomas
-
Hyperplastic polyps
-
Inflammatory polyps
-
Familial adenomatous polyposis, a rare hereditary disorder that causes hundreds of polyps in the lining of the colon beginning in the teenage years. If this is left untreated, the patient becomes high risk to develop colon cancer.
-
Hereditary nonpolyposis colorectal cancer, a hereditary disorder that causes an increased risk of developing colon cancer.
Your next task in coding is determining — without a doubt — if a polyp is benign or malignant. If you think you would find the clues in the pathology report (PR), think again. Usually, the PR will not use the term “benign” or “malignant.” However, it will use a description that points to the usual behavior of the polyp. It’s up to you to interpret those descriptions as benign or malignant.
Note: Even the gastroenterologists themselves usually defer to the pathology report before making a recommendation. “One of the quality measures your physicians will be reporting to CMS deals with the whether the patient was advised to return at the appropriate interval following a polyp removal,” says Michael Weinstein, MD, a gastroenterologist in Chevy Chase, Md., who is affiliated with multiple hospitals in the area. “They will want to get this interval correct based on the actual pathology report rather than their guess about the polyp type.” Hence an expert’s recommendation would be that you always wait for the pathology report to come back before deciding on a particular ICD-9 code for the patient.