NGS About to Up Some E/M Demands
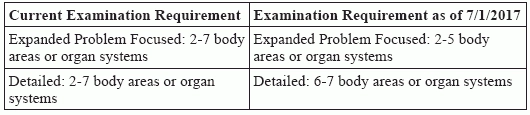
Detailed exams are about to level up. Recently, the Medicare Administrator Contractor (MAC) National Government Services (NGS) announced changes to its policy regarding evaluation and management (E/M) expectations for expanded problem focused and detailed exams. Let’s look at the NGS announcement and see what the CMS guidelines say about expanded problem focused vs. detailed exams. Change to Occur in July According to its announcement, the NGS change to E/M expectations for expanded problem focused and detailed exams will be effective for services that physicians perform on and after July 1, 2017. NGS included the following chart in its announcement. Check it out to fully grasp the changes: NGS initiated this change because multiple providers have asked for clarification about the current requirements for expanded problem focused and detailed exams, says the announcement. “Citing the same scope of examination for both levels has led to frequent provider confusion on documentation requirements and coding selections, as well as a degree of subjectivity in reviewing medical records for these services,” says NGS. “This change will eliminate the confusion and bring NGS into alignment with other CMS-sponsored review entities.” Check Out 1995, 1997 E/M Guidelines To better see the full impact of the NGS exam requirement change, let’s take a closer look at what the 1995 and 1997 Documentation Guidelines for E/M Services say. Similarities: Both the 1995 and 1997 guidelines base the levels of E/M services on four types of exams: problem focused, expanded problem focused, detailed, and comprehensive. Since the NGS announcement deals with expanded problem focused and detailed exams, see how the 1995 and 1997 guidelines define those types of exams: Per both the 1995 and 1997 guidelines, an exam can involve either several organ systems or one single organ system. “The type and extent of the exam performed is based on clinical judgment, the patient’s history, and nature of the presenting problem(s),” say both sets of guidelines. Differences: Although they share similarities, the 1995 and 1997 guidelines differ significantly when it comes to the E/M exam documentation requirements. 1995 Guidelines: According to the 1995 guidelines, the medical record for a general multi-system exam should include findings of eight or more organ systems. 1997 Guidelines: The 1997 guidelines describe the exam in more depth by differentiating between general multi-system and single organ exams. Coders Gain Clarity with Change Our pros weighed in on how the NGS change will affect E/M coders. “I think it is great that they are defining it for their providers who submit claims to them,” says Suzan Hauptman, CPC, CEMC, CEDC, senior principal of ACE Med group in Pittsburgh, Pa. After all, “it’s better to be transparent … Now [providers] have clear guidelines » » to be in line with the two different examination levels,” according to Hauptman. There will also be some challenges with the change. “This will be a significant change because the current requirements require not only 2-7 systems be examined, but for an EPF exam a limited exam of the affected body area or organ system, and for a detailed exam 2-7 systems with an extended exam of the effected body area or organ system,” says Marcella Bucknam, CPC, CCS-P, COC, CCS, CPC-P, CPC-I, CCC, COBGC, manager of clinical compliance with PeaceHealth in Vancouver, Wash. “It is the ‘limited exam’ and ‘extended exam’ portion of the rule that causes so much confusion.” These new requirements will have both a good and bad impact, according to Bucknam. “On the good side, it will be much easier to get a detailed exam for some specialties,” says Bucknam. “If you document even a very brief exam of at least six systems, you will be able to bill the higher-level service.” It will also be easy to count the exam elements and to know that your MAC agrees with that level of service, adds Bucknam. However, the change will also have a negative impact, according to Bucknam. “On the bad side, if you are in a specialty where you wouldn’t typically do an exam of lots of different parts of the body, but where you might do quite an extended exam of the specialty system and maybe one or two others, you won’t be able to bill a detailed exam using the 1995 rules,” says Bucknam. “Specialties like GI, cardiology, ophthalmology, dermatology, and others will be forced to use the 1997 specialty exams instead of the 1995 exams.” Bucknam further explains her thoughts. “The1997 rules are quite specific; there are some elements that are simply not included in the 1997 single system exams,” says Bucknam. “Providers in those specialties will have a steep learning curve to learn the requirements for the 1997 exams in order to bill the higher-level services.” Check with your payers: This change applies to NGS customers only, so other MACs may follow different rules. You should always check to see what your MAC expects and what rules you should follow. “Some MACs, like Noridian where I work, follow CPT® and the CMS guidelines exactly and don’t apply other standards,” says Bucknam. “Following NGS rules will not work for Trailblazers or Noridian or other MACs.” Also: “Novitas has their own exam guidelines that separates the detailed exam from the expanded problem focused exam,” explains Barbara J. Cobuzzi, MBA, CPC, CENTC, COC, CPC-P, CPC-I, CPCO, AAPC Fellow, Vice President at Stark Coding & Consulting, LLC, in Shrewsbury, N.J. “However, the Novitas exam is different from the new NGS guidance in that they require a ‘4x4 exam’ for detailed exams. The Novitas ‘4x4’ means that the provider must address four elements for four body areas/organ systems must in order to qualify for a detailed exam,” Cobuzzi continues. Bucknam adds that commercial payers and state Medicaid may not accept these special rules, so the practice may have to follow two sets of rules, depending upon the payer.