Rely on ROS Smarts for Coding Acumen

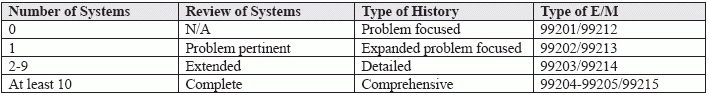
Remember, ROS has 3 levels. The review of systems (ROS) is a key component to many evaluation and management (E/M) services, yet coders can sometimes get confused by its intricate documentation. Knowing how many systems you need to count for the appropriate level of service, and knowing how you should document them in order to count, are just two of the problems all primary care coders face on a constant basis. So, if you're new to coding and you need a place to start, or if you just need a refresher on the ROS rules and regulations, the following answers to these frequently asked questions should help you evaluate and manage your own E/M coding skills. Q: What is an ROS, and Why Is It Needed? A: According to CPT® guidelines, the ROS "helps define the problem, clarify the differential diagnosis, identify needed testing, or serves as baseline data on other systems that might be affected by any possible management options." Essentially, according to Mary I. Falbo, MBA, CPC, CEO of Millennium Healthcare Consulting Inc. in Lansdale, Pennsylvania, "to guide a patient's E/M, you need a reasonably thorough ROS." Suzan Hauptman, MPM, CPC, CEMC, CEDC, AAPC Fellow, senior principal of ACE Med in Pittsburgh, agrees. "From a medical prospective," Hauptman notes, "a review of systems is needed to better understand the current condition of the patient. If a patient arrives with problem X," she adds, "and, although unrelated, has problem Y, the treatment options for X might be limited based on the Y." A thorough ROS will uncover such needed information. Q: What are the Systems, and How Many Should Provider Review? A: CPT® identifies a total of 14 systems that a provider can review during an E/M service: The number that should be reviewed depends on complexity of the history of the patient's present illness. The number then translates into the extent of ROS, which supports the type of history taken, which, in turn, helps determine the level of E/M service documented. Q: Does the ROS Have to Be Recorded by a Physician? A: No, it doesn't. In its Documentation Guidelines for Evaluation and Management Services, the Centers for Medicare and Medicaid Services (CMS) says that the ROS and/or the past, family, and/or social history (PFSH) can be performed by ancillary staff or the patient, who can "complete a form to provide the ROS and/or PFSH." However, if this is done, your practice "must provide a notation supplementing or confirming the information recorded by others to document that the physician reviewed the information." (Source: https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/Downloads/eval-mgmt-serv-guide-ICN006764.pdf). Or, as Hauptman puts it, "the ROS can be recorded by the patient or any clinical staff within the office; however, the provider's review of information obtained in the ROS must be evident within the record in order for the coder to use it toward the justification of the code. The important piece for the coder," Hauptman maintains, "is to be able to see the provider's review of the questions, the performance of the questioning, and/or the inclusion of that information in the note." Q: How Does the ROS Need to Be Documented? A: This can be one of the trickiest issues for coders for three reasons. First, according to Falbo, "some coders confuse past medical history with ROS. For example, if the provider documents, 'No known drug allergies,' this is past medical history and not ROS. To count as ROS," Falbo reminds coders, "the provider would need to document something like, 'no wheezing,'" which would count as a review of the respiratory system. A second point of confusion for coders can arise over whether negatives should be included in the review. Falbo suggests providers "document both positive and negative findings for any pertinent system." So, a review of the gastrointestinal system for a patient complaining of chest pains could include notes about negatives, such as "No complaints of nausea, vomiting, or change in stool pattern, consistency, or color," as well as positives such as "Burning epigastric pain at night, approximately twice a month." Coders should also note that an extended or complete ROS can include reviews of systems that are not directly related to the problems identified in the history of present illness (HPI). In the above example of the patient complaining of chest pains, you could count a review of the ears, nose, mouth, and throat if your provider documented that the patient had "no complaints of headache, change in vision, or problems with the nose or ears." In other words, "something needs to be documented," according to Falbo, "in order to count toward the E/M level of service." Simply put, Hauptman concludes, "it is important to have evidence that the review took place."