Solve These Subsequent Care Scenarios

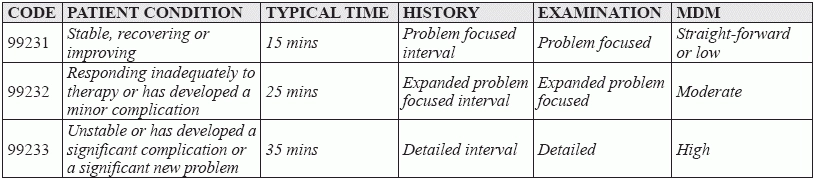
Let our experts help you evaluate and manage service level determinations. When a provider is called upon to provide care for one of your patients following a hospital admission, coders know they should immediately flip to the 99231-99233 (Subsequent hospital care, per day, for the evaluation and management of a patient …) codes in their CPT® manuals. But assigning the correct code for the level of service can be an intimidating task. Why? Like most evaluation and management (E/M) services, coding subsequent care requires you to apply an elaborate formula based on the level of history taken, the detail of the exam, and the complexity of the medical decision making (MDM). And as if that wasn’t enough, the subsequent care codes also involve some subtle guideline differences as well. But there’s no need to be confounded. Simply spend some time with these scenarios and let our experts’ analysis help you code subsequent care services with care. Breaking Down the Codes Like other E/M codes, 99231-99233 describe increasingly severe medical conditions and an increasing amount of work on the provider’s part to treat them. Each also describes an increasing amount of typical time spent at the bedside and on the patient’s hospital floor or unit. On the patient side, the conditions range from the lowest level, where the patient is stable, recovering, or improving, to the highest, where the patient is unstable and getting worse because he or she has developed a significant complication or a significant new problem. On the provider side, the codes reflect reviews of the condition’s history, an examination of the patient, and level of medical decision making (MDM) appropriate for treating the patient. From the provider’s perspective, the codes follow similar guidelines to many of the other E/M codes. Two of the three key components — history, exam, and MDM — need to be present in the documentation to support the level of service if coding on that basis, and if MDM is one of those components, two of three MDM components (number of diagnoses/management options; amount or complexity of data to be reviewed; or risk of complications and/or morbidity or mortality) need to be present to determine the level of MDM complexity. Both sides of this E/M equation can be summarized in the following table. What are the Similarities and Differences Between 99231-99233 and Other E/M Codes? The main difference is in the level of history taken. CPT® describes it as an “interval” history, which is basically a history of the patient’s condition since the last time the patient was seen. This means, as the Centers for Medicare and Medicaid (CMS) puts it, “it is not necessary to record information about the PFSH [past family and social history]” (Source: https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/Downloads/eval-mgmt-serv-guide-ICN006764.pdf).