Practices Shorted Themselves Nearly $210 Million in Downcoded E/M Visits Last Year

CERT results reveal that insufficient documentation topped list of Part B errors last year.
With all the talk about the OIG coming after you for upcoding errors, it can be easy to forget that downcoding is a problem for many practices as well. And the latest CMS Comprehensive Error Rate Testing (CERT) results show that medical practitioners left over $1 billion on the table by undercoding claims in 2015.
CMS’s new CERT results, which were released last month, show that practices forfeited $209.3 million alone just by downcoding established patient office visits (99211-99215). If you’re downcoding your office visits, you’re not only abandoning money you’ve earned, but you’re also coding incorrectly since your documentation must support the level of service you’ve chosen to bill.
Also among the most commonly downcoded services were coronary bypasses without cardiac catheterization, nursing home visits, subsequent hospital visits and major joint replacements, among others. In total, practices forfeited $1.17 billion last year thanks to downcoding errors.
To avoid this issue, always determine the criteria for the service you’ve provided, and then select the most accurate code based on the documentation. As long as your records support the code, you shouldn’t be worried about sometimes billing a higher code than you’re accustomed to reporting.
Other Problems Plagued Part B Claims as Well
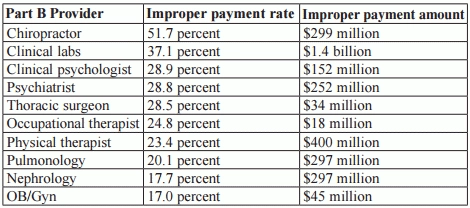
Overall, Part B practices had $11.5 billion in improper payments last year, both due to undercoding and overcoding. Among the big culprits were lab tests, which logged a 39.0 percent error rate, initial hospital visits, which saw a 19.1 percent error rate, and chiropractic visits, which were billed improperly a whopping 51.7 percent of the time.
Documentation: The majority of the errors that CMS found involved insufficient documentation, which comprised 65.4 percent of the incorrect payments. The next most common issues were medical necessity errors (19.7 percent), incorrect coding (10.5 percent) and no documentation (1.3 percent).
Allergists, Pain Management Specialists Logged High Error Rates
The CERT report indicates that allergy/immunology specialists had some of the highest improper payment rates among Part B practices at 27.5 percent, along with interventional pain management specialists who logged a 21.6 percent error rate. The following list shows other Part B providers with high rates of error:
Resource: To read the complete CERT results, visit www.cms.gov/Research-Statistics-Data-and-Systems/Monitoring-Programs/Medicare-FFS-Compliance-Programs/CERT/CERT-Reports-Items/Downloads/AppendicesMedicareFee-for-Service2015ImproperPaymentsReport.pdf