Find Out If Your Part B Pay Will Increase in 2018

Don't expect the conversion factor's slight bump to make much of a difference next year. If you thought Medicare's annual revaluation of codes would bring a big boost to your practice's bottom line in 2018, think again. New CMS guidance slows down past policy changes and offers relief to overburdened practices; however, for most Medicare Part B providers, it will be business as usual. Look at the Conversion Factor Physicians can expect a slight increase this year with the conversion factor going up from $35.89 in 2017 to an estimated $35.99 for 2018. However, this miniscule rise in the conversion factor is more of a "budget neutrality adjustment," explains the Medicare Physician Fee Schedule (MPFS) final rule. Reminder: The MPFS establishes different values for codes depending on the setting/site (facility or non-facility) in which the provider performs the service or procedure. For some services, the total RVUs for a given procedure are the same in a facility or a non-facility setting. In some cases, however, the two totals may differ. Remember that to calculate the fee for a Medicare service, you'll multiply the conversion factor by the total relative value units (RVUs). For instance, CPT® code 99213 (Office or other outpatient visit for the evaluation and management of an established patient, which requires at least 2 of these 3 key components...) currently has a total RVU of 2.06 for 2017, which comes out to a fee of $73.93 when multiplied by the 2017 conversion factor of $35.89. If, however, you want to see how much more or less you'll make according to changes in the conversion factor from 2017 to 2018, you'd then figure out the geographically unadjusted Medicare fee for 99213, multiply the transitioned non-facility total (2.06) by $35.99. You can therefore see that the 2018 unadjusted fee for the E/M service is $74.14 - a positive change of 21 cents. Consider this: "Medicare had indicated there would be a 0.5 percent increase in reimbursement in 2018. However, due to various offsets and budgetary restraints the conversion factor in 2018 is $35.99 vs. $35.89 in 2017," reminds Vinod Gidwani, founder and president of Currence Inc. in Skokie, Illinois (medcurrence.com). "This amount is about half of the promised 0.5 percent." "Additionally, some specialties like allergy, otolaryngology, and others will see a cut of 1 percent to 3 percent," Gidwani warns. While "primary care [will be] among the few big 'winners,' promises made are not necessarily promises kept." Rundown: As CMS steadies itself and revises MACRA-backed ideologies for the Quality Payment Program (QPP) Year 2, value-based, incentivized care that puts the patient first continues to influence policies, payments, and fees. This approach is evident in the 2018 MPFS and is specifically highlighted in the estimated impact on total allowable charges in the Federal Register report. Who Came Out Ahead and Who Fell Behind Clinical social workers and other behavioral health specialists lead the pack with an estimated combined impact of 3 percent while diagnostic testing facilities look to see the biggest declines. Here's a glance at some of the biggest impacts on specialties and their estimated increases and decreases for the CY 2018: Status quo: A majority of providers will see very little difference to their 2018 Medicare pay due to the limited changes of next year's estimated fees. But the impact of the revaluation of codes and services under the final rule may affect other areas of practice administration. Tip: CMS offers providers and their billing staffs tools to investigate the revaluations. You can simply look up national or local Medicare reimbursement rates for specific procedures on the Medicare website at www.cms.hhs.gov/PFSlookup, or on https://www.aapc.com/codes/. Many individual Medicare carriers also have similar web tools.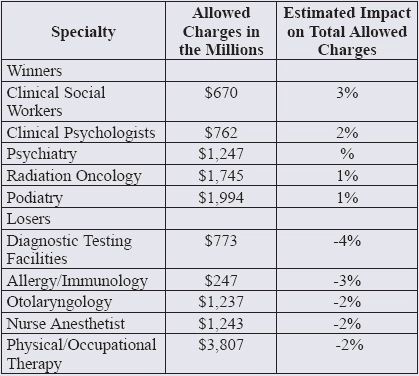
(Data from TABLE 50: CY 2018 PFS Estimated Impact on Total Allowed Charges by Specialty in the Federal Register on Nov. 15, 2017)




