Straightforward Crosswalk Helps Pinpoint Actinic Keratosis Diagnoses
Under ICD-10, L57.0 will be your go-to code.
When your clinician diagnoses actinic keratosis, you report the condition in much the same way as you did in ICD-9. You also have a simple crosswalk code to clinch the diagnosis in ICD-10.
ICD-9: When your practitioner arrives at a diagnosis of actinic keratosis, you report 702.0 (Actinic keratosis). You cannot use 702.0 when the provider confirms the diagnosis as carcinoma in situ. This has to be reported from the ICD-9 code range 232.0-232.9 instead.
Also, you cannot use 702.0 when your clinician diagnoses any skin conditions that are congenital. These have to be reported using the ICD-9 code range, 757.0-757.9. Again, a condition that is confined to the eyelids cannot be reported using 702.0. These are reported with the ICD-9 range 373.0-374.9.
ICD-10: A diagnosis of actinic keratosis that you report with 702.0 in ICD-9 crosswalks to L57.0 (Actinic keratosis) in ICD-10. You will use the same diagnosis code if your clinician’s diagnosis mentions the condition to be senile keratosis, solar keratosis, or keratosis NOS.
Focus on These Basics Briefly
Your physician will arrive at a diagnosis of actinic keratosis based on a complete history and an evaluation of the person’s signs and symptoms. The condition occurs almost exclusively in fairer skinned patients who are exposed to prolonged periods of sunlight.
Your clinician will note the presence of multiple small lesions on the skin that are more easily felt (sand paper-like texture) than visibly distinguished. The documentation will most likely indicate that these lesions are found occurring on areas of the skin that are exposed to the sunlight (for instance, face, lips, neck, ears, chest, hands, forearms, and sometimes scalp). The lesions are small and measure less than a centimeter in size, although your clinician might note that some lesions are larger.
These lesions are typically red and have a scaly appearance, and the skin around each is pale and appears hyperpigmented with deep wrinkles. Most of the lesions will be asymptomatic, although it is possible that sometimes there can be some itchiness or bleeding in the affected area.
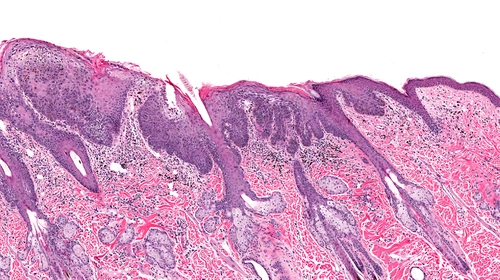
Tests: Your physician will not typically conduct any blood tests if he suspects a diagnosis of actinic keratosis. Instead, he will resort to obtaining a biopsy of the lesion. The biopsy will not only help your clinician to confirm a diagnosis of actinic keratosis, it will also help your doctor rule out other conditions, such as squamous cell carcinoma.
Apart from this, your clinician might also perform a fluorescence test wherein a photosensitizing drug such as methyl ester of 5-aminolevulinic acid [ALA] and a photodynamic therapy lamp or a wood lamp is used. When the lamp is held over the affected area, it will emit a pink fluorescence which will help confirm the diagnosis of actinic keratosis.
Based on history, signs and symptoms, and results of the fluorescence tests and biopsy, your clinician will be able to confirm a diagnosis of actinic keratosis.
Example: Your clinician reviews a 63-year-old male, white patient with complaints of skin eruptions on the scalp area and the neck. The patient is a new patient and has not been to your practice before. The patient complains that he has been having these eruptions for a long time in the past but they have become itchy and have a tendency to bleed within the past month or so. The patient’s occupational history reveals that the patient was a construction worker for many years previously.
Upon examination, your clinician notes multiple skin lesions in the scalp and neck area that have a rough, sandpaper-like texture when palpated. He notes that some of the lesions are easily visible to the eye, although many lesions are not easily distinguished visibly. He also notes that some of the lesions in the neck area are bleeding slightly.
Your clinician then performs a fluorescence test to confirm the diagnosis of actinic keratosis. Since some of the lesions show signs of bleeding, he obtains a biopsy to rule out invasive lesions such as squamous cell carcinoma. The results of the biopsy confirm your clinician’s suspicion of actinic keratosis and help rule out squamous cell carcinoma.
What to report: You report the diagnosis of actinic keratosis with 702.0 if you are using ICD-9 codes or report L57.0 if you are using ICD-10 codes. You report the evaluation of the patient with an E/M code such as 99203 (Office or other outpatient visit for the evaluation and management of a new patient…) and the skin biopsy procedure with 11100 (Biopsy of skin, subcutaneous tissue and/or mucous membrane [including simple closure], unless otherwise listed; single lesion). If he biopsied more than one lesion, you report the additional biopsies with +11101 (…each separate/additional lesion [List separately in addition to code for primary procedure]).

