Know How to Mix HPI/Exam for E/M Calculations

Some payers now allow you to use crossover elements.
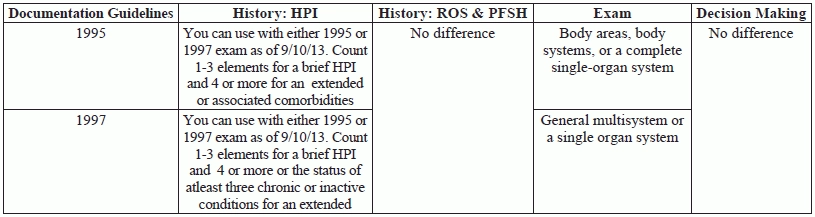
Calculating the level of evaluation and management (E/M) service your physician provides can be a challenge because of all the components. Add in two sets of guidelines — the 1995 and 1997 guidelines — and the confusion mounts. When it comes to using a patient’s history of present illness (HPI), review of systems (ROS), and past medical, family, and social (PMFSH) histories to choose the historical component of the service, things have gotten easier.
For some payers, you can now use the HPI criteria from either the 1995 or the 1997 Documentation Guidelines for Evaluation & Management Services. This allows the ability to now “mix” the best history with the best physical examination to determine the level of service, and will give your provider more options for meeting the level of service.
Here’s a look at the change and how you can use this change to make your job, and your provider’s job easier.
Refresh Your 95 vs. 97 HPI Knowledge
The HPI describes the development of a patient’s present illness from the first sign and/or symptom or from the previous encounter to the present encounter. 1995 way:
Under the 1995 guidelines, to assess the level of HPI, you count the number of HPI elements the provider reviewed and documented. The guidelines include eight elements:
1. location
The medical record should describe one to three elements for a brief HPI. For an extended HPI, the medical record should describe four or more elements or associated comorbidities. You can count comorbidities in past history, ROS, or HPI.
1997 way: With 1997 guidelines, you choose a level of HPI based on the number HPI elements documented as you did above for the 95 guidelines or the number of chronic or inactive conditions your provider reviews with the patient. A brief HPI consists of one to three elements or status of one to two chronic or inactive conditions. An extended HPI consists of at least four elements or the status of at least three chronic or inactive conditions.
Get to Know the Change
Thanks to the guidance from CMS and HHS, you can now mix and match the 1995 and 1997 guidelines for counting HPI with the physical examination and MDM.
“Beginning for services performed on or after September 10, 2013 you are able to use the 1997 documentation guidelines for an extended history of present illness along with other elements from the 1995 guidelines to document an evaluation and management service,” announced CMS and HHS.
In other words: For services your physician has performed since September 10, 2013, you may use the 1997 documentation guidelines for HPI along with the physical examination criteria from the 1995 guidelines, or vice versa, using the 1995 HPI criteria with the 1997 examination guidelines.
In the past, you had to pick either 1995 or 1997 guidelines and apply your choice to the entire encounter. But now, you can use either the status of inactive or chronic conditions or the HPI elements for the history and still choose either the 1995 or 1997 guidelines for the physical examination portion of the encounter.
This change may make your job easier when you are reviewing your provider’s documentation and determining the best code to assign. “I find it beneficial in that providers may have been trained to document using either of the documentation guidelines,” Lynn M. Anderanin, CPC,CPC-I, COSC, ICD10, is the sr. director of Coding Compliance and Education for Healthcare Information Services in Park Ridge IL. “When auditing records, I can usually recognize which they are using. This allows me to able to use either/or to justify the level of service. Often, the 1995 guidelines for examination are easier to obtain than the 1997 guidelines, especially in the higher levels of service.”
“If the physician is a specialist, there might be times that the examination is targeted to the specific organ system, but there may be other times when a more general exam is warranted,” explains Suzan Berman (Hauptman), MPM, CPC, CEMC, CEDC, manager of physician compliance auditing at Allegheny Health Network in Pittsburgh, Penn.
Pointer: Medicare contractors such as First Coast Service Options, Inc. (medicare.fcso.com/faqs/answers/197576.asp) and Noridian Healthcare Services (med.noridianmedicare.com/web/jeb/specialties/em) have announced they will recognize either the 1995 or 1997 guidelines for the HPI no matter which guidelines were used for the examination. Make sure you check with your payers to see if they will recognize this guidance.
Clarify the HPI Guidelines Change with an Example
Take a look at the following office visit scenario to see how the HPI/examination mixing option can help you reach a higher level of service in some cases.
Details: An existing 52-year-old male patient comes to see your physician. Your provider documents a chief complaint, 10 systems reviewed in review of systems, and complete past medical, family, and social history. For HPI he writes the following: “Patient’s labs show that his PSA is still running high despite medication. Wants change in medication as Lupron isn’t covered by his insurance. Patient’s hypertension is stable. He takes his blood pressure at home and I have reviewed his numbers for the last 30 days. Medications have not caused BP increases. Patient’s blood sugar readings for the past 30 days also look good. Diabetes appears stable.” For the exam, your physician documents the patient’s vital signs and also writes: “Patient is oriented times three, looks well. Lungs sound clear. Heart sounds normal. Eyes PERRLA. Abdomen soft, non-tender. Testes appear normal. Prostate slightly enlarged. No edema. No rashes; skin clear.” The provider then documents moderate complexity MDM due to review of multiple chronic conditions (benign prostatic hyperplasia, hypertension, and diabetes), various tests being reviewed and ordered, and medication adjustments that raise the risk to moderate.
Start counting: When using 1995 HPI guidelines, you get brief HPI due to only three elements — location, severity, and modifying factors. Under 1995 guidelines, you can count a comprehensive exam because the provider documented examination of eight systems.
Under 1997 guidelines, you can count an extended HPI because the provider gives the status of three chronic conditions. For the exam, however, you will only get an expanded problem-focused exam under 1997 guidelines because the provider only mentions nine bullets from the general multi-system specialty exam guidelines.
If you use the 1995 HPI and exam, your code level will be 99214 (Office or other outpatient visit for the evaluation and management of an established patient, which requires at least 2 of these 3 key components: a detailed history; a detailed examination; and medical decision making of moderate complexity …) due to expanded problem focused history, comprehensive exam, and moderate MDM. With 1997 HPI and exam, you get 99214 as well due to comprehensive history, expanded problem focused exam, and moderate MDM.
New way: Now that you can mix and match the guidelines, your best bet for this encounter would be to combine the higher 1997 HPI to the other complete components of the history and the higher 1995 exam guidelines. That gives you comprehensive history, comprehensive exam, and moderate complexity MDM. This technically supports a 99215 (Office or other outpatient visit for the evaluation and management of an established patient, which requires at least 2 of these 3 key components: a comprehensive history; a comprehensive examination; and medical decision making of high complexity …).
Important: Be cautious, however, and be sure the medical necessity warrants 99215. The overriding criterion for coding an encounter is medical necessity and in the example, the need for the complete history and comprehensive exam is illustrated by the chronic illnesses. The 99215 is thus the billable level of service for this scenario.
2. quality
3. severity
4. duration
5. timing
6. context
7. modifying factors
8. associated signs and symptoms.