Bipartisan Budget Act Slims Some MIPS Requirements
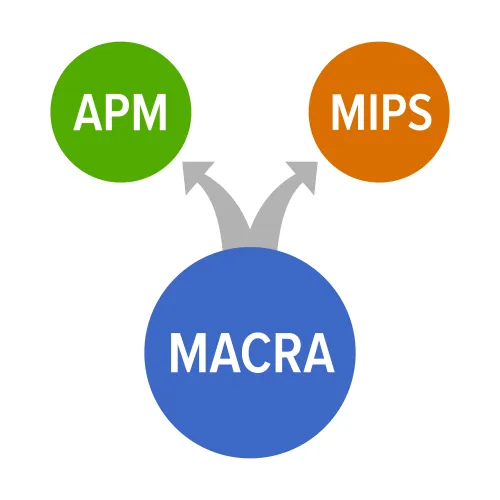
Cost category percentages could remain status quo, BBA suggests As the dust settles on Performance Year 1 of the Quality Payment Program (QPP), Part B providers are heaving a sigh of relief. And, though the calculations aren't in yet on whether Medicare's reimbursement opus was a success, the government has already decided to reduce some requirements in 2018 and beyond. Context: MACRA mandated a replacement for the Sustainable Growth Rate (SGR) system that supported value and quality care. The new QPP was initiated in 2017 under two distinct Medicare reimbursement paths - the risk-and-reward Advanced Alternative Payment Model (APM) and the entry-level Merit-Based Incentive Payment System (MIPS). Throughout the first year of its implementation, CMS cut MIPS requirements for eligible clinicians to make reporting quality measures easier, hoping to ensure physician adoption of the new system. Once underway, MIPS was met with a mix of understanding, consternation, and a little confusion. After the Federal Register published a final rule on the QPP Year 2 changes last November, many were relieved to see MIPS trimmed and made more manageable for Part B providers. However, deregulation has been the feds theme song these last 12 months, and practices hoping for more reductions can sing a happier tune. See the Bipartisan Budget Act Updates Here The Bipartisan Budget Act of 2018 signed by the President in February has a few MIPS gems hidden deep in its content, suggests attorney Elizabeth N. Pitman, CHPC of Waller Lansden Dortch & Davis, LLP out of the Birmingham, Alabama office in a Waller Healthcare Blog post. "Congress rolled out several changes with potentially big impact on physicians and providers." Take a look at the top four Budget Act impacts reshaping MIPS in the years ahead: Consider this: The Budget Act changes support current trends at CMS to reduce burdens, putting patient care first. With Patients Over Paperwork initiatives at the forefront of everything Medicare, expect more cutbacks and turnovers like these in the months ahead. Note: See the Budget Act text at www.congress.gov/bill/115th-congress/house-bill/1892/text#toc-H7C43975019384EE2B2D44BE44671B479.