Compare Your Physician Assistant's Modifier 25 Billing with Other PAs

Take a look at a recent CBR on physician assistants, E/M visits, and modifier 25.
Benchmarking has become a popular revenue tool for providers to compare their billing patterns against those of their medical cohorts. Sifting through the data to see where you rank can help your practice figure out the ups and downs of billing trends, revenue, and more importantly, your level of patient care.
Background. The OIG took a random sampling of 450 claims out of 29 million in 2002 and discovered that modifier 25 (Significant, Separately Identifiable Evaluation and Management Service by the Same Physician or Other Qualified Health Care Professional on the Same Day of the Procedure or Other Service) was commonly abused, costing CMS millions.
“The OIG found 35 percent of the services provided did not meet Medicare program requirements, which resulted in improper payments of $538 million,” said Tamara Canipe RN, clinical quality management coordinator with Palmetto GBA CBR in a recent webinar. “OIG also found that a large number of claims with modifier 25 were appended, when no other service was performed on the same day. While the claims were not overpaid, they were filed incorrectly.”
Palmetto GBA’s CBR Group Acts on OIG Study
Due to the scope of incorrectly billed claims with modifier 25 and the excessive improper payments paid out, Palmetto GBA’s Comparative Billing Reports (CBR) group, in coordination with eGlobal Tech, released CBR 201611, which compared the data of over 12,000 Medicare Part B providers who billed for established patient E/M visits performed by physician assistants (PAs) when modifier 25 was appended. The CBR aims to address the issues with modifier 25 and analzye trends when it is used with five different CPT® codes related to PAs.
Problems with modifier 25. “Modifier 25 is a CPT® modifier and should only be appended to an E/M service,” Canipe explained, and herein lies the issue. Across the spectrum of the studies at both OIG and within different state agencies, Palmetto GBA found disparities and confusion related to things like subspecialties, global periods, and using modifier 25 “when no other conditions were serviced.”
PAs cannot report using subspecialties, and each state and MAC determines what services they will cover, suggests CBR 201611, which also references this MLN booklet on services covered by Medicare for PA care, https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/Downloads/Medicare-Information-for-APRNs-AAs-PAs-Booklet-ICN-901623.pdf. The CBR reminds practices to thoroughly take into account incident-to as well since this needs to be properly coded for some PA care.
Here is the Global Surgery Caveat
Another factor Palmetto GBA unearthed in its research concerns global days, and how these distinct periods affect appending modifier 25. Distinguishing between minor and major procedures can be tricky, but checking the global surgery packages will help you avoid modifier 25 problems.
Minor service. For example, a patient comes in for a simple splinter removal, but while in the office, she presents with high blood pressure due to the fact that the medicine she takes makes her feel sick, and she’s stopped taking it. You prescribe a new medicine for the blood pressure issue and send the patient on her way. This case is a minor procedure under the 000-010 global days period, and it can be billed as an E/M service attaching modifier 25, says Canipe.
Major procedure. The next level of care at, say, a 090-day global surgery package will likely be more serious, she advises. “For example, a patient falls and comes to the office with a broken hip, and the doctor decides to do surgery that same day. That would be an E/M service with modifier 57 (Decision for Surgery).”
“Modifier 25 should be reserved for the unexpected,” Canipe explains. She goes on to clarify that documentation is key, and the notes must clearly state that to use modifier 25 the service must be a “stand alone” issue. Here is a quick reference guide Palmetto GBA mentions, devised by the American Academy of Family Physicians (AAFP) to ensure you are billing this correctly:
How They Garnered the Results
With separate research at both the state and national levels, CBR 201611 looks at 12,000 providers’ claims, utilizing NPI, specialty 97 for physician assistants, and the CPT® codes 99211-99215 with or without modifier 25. The data was extracted on June 13, 2016 from the CMS Integrated Data Repository (IDR) and covers the dates of service from Jan. 1, 2015 to Dec. 31, 2015.
As with previous CBRs, the benchmarking details allow for four possible outcomes: your billing results are significantly higher than your peers, higher than your peers, equal to your peers, and/or your results are inconclusive due to the lack of sufficient individual data, suggests the eGlobal Tech representative in the webinar. Two peer groups were outlined in the results: PAs at the state level were evaluated with CPT® codes 99211-99215 and PAs at the national level with CPT® codes 99211-99213.
Consider these equations. To get its results, eGlobal Tech used a variety of equations to measure the metrics related to the codes and modifier 25 at the state and national levels, finding the averages for how many times modifier 25 was or was not used with the CPT® codes, the average allowed minutes, and the average allowed charges per beneficiary.
To figure out the averages of how often providers used the codes with modifier 25, the researchers took the “total number of services with modifier 25 divided by the total number of services and then multiplied by 100,” the CBR fact sheet states.
Time matters. The CBR report suggests to providers who’d like to find where they rank in allowable minutes to divide their total E/M weighted services (with or without modifier 25) by the total number of E/M visits (with or without modifier 25). The national average of allowable minutes per visit for a PA appending modifier 25 with CPT® codes 99211-99213 was 18.03 minutes versus 18.61 minutes for the defined E/M services without modifier 25. There was a tie between New Mexico and North Dakota for the top spot with an average time of 20.64 minutes with modifier 25 while Utah ranked first for care with it.
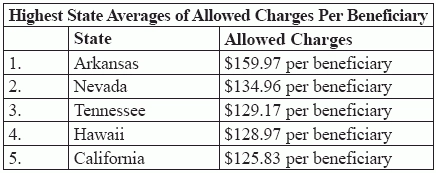
Here are the Top 5 States with the Most Allowed Charges Per Beneficiary
The study highlighted that the national average for allowed charges per beneficiary was approximately $108.47. The CBR report shows that they found the averages by dividing the total allowed charges by the total number of beneficiaries.
Here is a look at the top 5 states with the most allowed charges per beneficiary:
*Data from CBR 201611 by Palmetto GBA CBR and eGlobal Tech. CBR201611 Average Allowed Charges per Beneficiary.xls.
Endnote. If you rank in the middle or on the higher end, there is not necessarily anything to worry about, and the benchmarking results can help you determine how you figure into the grand scheme of things. However, “if your billing differs significantly, it might be necessary to do a self-audit to figure out why,” says Canipe.
Resource: For more information on CBR 201611, visit http://www.cbrinfo.net/cbr201611.