Reevaluated GI Procedures Make Coding Moderate Sedation Easy

Be on the lookout for these six exclusive codes in 2017.
Your endoscopy reimbursement could look a lot different next year, thanks to the proposed Medicare Physician Fee Schedule (MPFS). The reason is that CMS plans to remove the value of moderate sedation from your GI endoscopy codes, starting Jan. 1.
Impact: “This will have a big impact on our physicians who do these types of scopes frequently,” says Lisa Center, CPC, Physician Practice Manager,Via Christi Hospital Pittsburg, Inc. Pittsburg, KS. “Their RVU totals will drop with the removal of the sedation component from the code.” Read on to know more.
Background: You’ll find more than 400 diagnostic and therapeutic procedures, in which moderate sedation is an inherent part of the procedure, as per the CPT® Editorial Committee guidelines. Therefore, the RVU costs of moderate sedation have always been included within the CPT® procedure, and merely reporting the procedure code is all that is required.
The whole issue: However, in the 2015 PFS proposed rule, CMS noted that many practices were reporting anesthesia separately from the endoscopy procedure codes. In CY 2016 PFS proposed rule (80 FR 41686), CMS again raised the issue that providers are now reporting a separate anesthesia service more than 50 percent of the time while reporting colonoscopy procedures.
“Since we believe that gastroenterologists furnish the highest volume of services previously identified in Appendix G, and services primarily furnished by gastroenterologists prompted the concerns that led to our identification of changes in medical practice and potentially duplicative payment for these codes, we have addressed the variations between the GI and other specialties in our review of the new moderate sedation CPT® codes and their recommended values,” says the proposed Medicare Physician Fee Schedule (MPFS) for 2017.
“Historically, GI physicians administered a combination of narcotics (meperidine or fentanyl) and a benzodiazepine (midazolam or valium) with nurses monitoring the patient,” explains Michael Weinstein, MD, former representative of the AMA’s CPT® Advisory Panel. “The majority of procedures are now done with Propofol sedation eliminating the risk of narcotic side-effects and achieving a faster recovery. However, Propofol must be administered by a provider trained in methods of general anesthesia (CRNA or Anesthesiologist) who will submit a claim for their own service.”
CMS’s woeful remedy: To establish uniformity as well as appropriate evaluation of the procedure codes in light of apparent changes in medical billing practice of all these appendix G procedures, CMS has proposed reworking the values of the procedure codes where moderate sedation had been inherently reported to begin with.
“Our providers don’t provide the sedation themselves; they are provided by anesthesia providers, so this will probably more accurately reflect the work RVU that they are performing with each code,” Center says.
New CPT® Codes Draw the Line
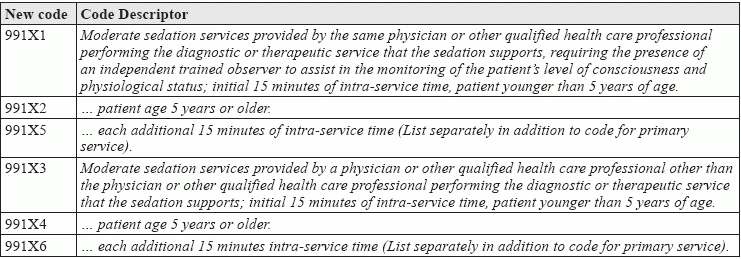
For 2017, the CPT® Editorial Panel has created six new codes and proposed elimination of Appendix G. As per this change, you would get payment for moderate sedation services only in cases where you provide the service and claim for it as well. The codes are:
The section II.L further explains about the new CPT® codes, along with how to align these new moderate sedation code with an existing endoscopy-specific moderate sedation code, as well as proposed evaluations demonstrating the variation in the physician survey data between other specialties versus gastroenterology.
In other words: This means that payment for your GI endoscopy procedures will come down further if you or your other provider do not provide moderate sedation.
How Does the Recalibration Work Out?
As per the recommended methodology, the RVS Update Committee (RUC) would eliminate the work RVUs related to moderate sedation from the Appendix G codes, following an evaluation of the codes to determine if providers perform the requisite procedure on typical uncomplicated patients or on patients that require greater care.
“From the provider’s perspective, this will not be a good thing, as this will directly impact the amount of RVUs they bring in with each scope,” Center says. “I feel that it is appropriate to do, however, since the code previously included RVUs for moderate sedation and our providers don’t do that part of the service.”
Keep a Close Watch on Potentially Misvalued Codes 00740 and 00810
CMS identified CPT® codes 00740 and 00810 are used for anesthesia furnished in conjunction with lower gastrointestinal (GI) procedures.
“Given the significant change in the relative frequency with which anesthesia codes are reported with colonoscopy services, we believe the relative values of the anesthesia services should be re-examined,” CMS says, in the proposed Medicare Physician Fee Schedule (MPFS) for 2017.
“We proposed to identify CPT® codes 00740 and 00810 as potentially misvalued and sought public comment regarding valuation for these services.”
However, as the current surveys do not provide appropriate representation of data, the RUC has recommended maintaining a base value of 5 for both these codes on an interim basis. These codes will be resurveyed with updated patient vignettes in near future, so that after incorporating input from specialty providers and others, CMS may be able to firm things up for a future rulemaking in this regard. “The survey for these codes will be performed amongst the providers who perform the services, the CRNA and Anesthesiologist communities,” informs Weinstein.
What Does All This Mean for GIs?
Changes Jeopardize 80 by 2018
According to the American Gastroenterological Society, these changes may impact the “80 by 2018 pledge.” This is a national drive with an aim of getting at least 80 percent of eligible beneficiaries screened for colorectal cancer by 2018.
The AGA is also critical of appropriate valuation of moderate sedation, so that the value of the endoscopy procedures is preserved. In case too much value goes in to moderate sedation, the underlying endoscopic procedure may get devalued.
Beware of the timelines: Comments on the rule must be submitted by Sept. 6, 2016. The final MPFS is typically released around Nov. 1. “Our providers will notice the impact in 2017 when this change goes into effect, and having a conversation prior to that is a must,” Center warns. “They must be kept in the loop about the changes coming so that it will not surprise them when they see their numbers drop.
For more information, check out the “Physician Fee Schedule 2017 Proposed Rule Potential Impact on Moderate Sedation” at https://www.gastro.org/practice-management/reimbursement/2017_MPFS_Proposed_Rule_Moderate_Sedation_-_Q-A.pdf.