Know Which Modifier to Add When You Report G-Codes
Get the latest CMS guidance.
Have you been puzzling over whether you need to include a modifier when reporting functional limitation G-codes in the 8978 to 9895 range? Our experts have advice for you.
Background: Reporting functional limitation codes, also known as G-codes, became mandatory effective July 1.
To whom does it apply? Specifically, the policy applies to physical therapy, occupational therapy, and speech-language pathology services furnished in hospitals, critical access hospitals, skilled nursing facilities, comprehensive outpatient rehabilitation facilities, rehabilitation agencies, home health agencies (when the beneficiary is not under a home health plan of care), and private offices of therapists, physicians, and nonphysician practitioners.
G-codes are “Always Therapy” codes which require a therapy modifier, Pamela R. West, DPT, MPH, of the Centers for Medicare & Medicaid Services, Center for Medicare Hospital and Ambulatory Payment Group, Division of Practitioner Services, said during a National Provider call in Dec. 2012.
She went on to add that each functional G-code set contains:
Current status
Projected Goal Status
Discharge Status
Gear Up for 2 Sets of Modifiers
To accurately report modifiers for the functional limitation G-codes, you’ll need to go the extra mile. Two sets of modifiers are required for this code range according to Rick Gawenda, PT, president of Gawenda Seminars & Consulting Inc.:
1. The severity/complexity modifier
2. The therapy discipline specific modifier (i.e. GN, GO, GP) for outpatient therapy.
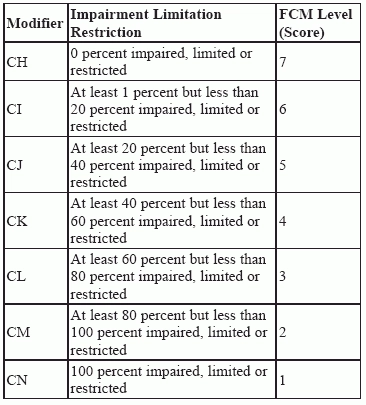
This table from the Centers for Medicare & Medicaid Services’ (CMS) should be used to indicate the severity modifiers:
The severity modifiers listed above reflect the beneficiary’s percentage of functional impairment as determined by the therapist, physician, or NPP furnishing the therapy services. You must report a severity modifier with each functional G-code
Use Guidelines for Selecting the Severity Modifier
The “C” severity modifiers reflect the score from a functional assessment tool or other performance measurement instrument, as appropriate. Use CMS’ guidance below.
Apply These Beneficiary Requirements
Keep in mind that claims submitted for outpatient (and CORF) PT, OT, and SLP services must contain the information on beneficiary functional limitations.
Medicare Claims Processing Manual, chapter 5, section 10.6 states that functional reporting is required on claims throughout the entire episode of care. And, generally only one functional limitation should be reported at a time.
However, you will report a second functional limitation for some beneficiaries.
For instance, when the beneficiary has reached his or her goal or progress has been maximized on the initially reported functional limitation, but the need for treatment continues, you must report a second functional limitation using another set of G-codes. So, for these beneficiaries, you’ll report two or more functional limitations during one therapy episode of care.
When do you need capture data about the beneficiary’s functional limitations? You should include non-payable G-codes and modifiers on the claims forms (a) at the first session; (b) at a minimum every 10th visit; and (c) at discharge, under this new rule, says APTA on its website.
Bottom line: You may need to report on more than one functional limitation for some patients, but not simultaneously.
Review Therapy Cap Exceptions
When the beneficiary qualifies for a therapy cap exception, you must add a KX modifier to the therapy HCPCS subject to the cap limits. Don’t add the KX modifier to any line of service that is not a medically necessary service. This applies to services that, according to a Local Coverage Determination by the contractor, are not medically necessary services. The KX modifier is in addition to therapy modifier GO or GP, and you should add it to each line of the claim that contains a service that exceeds the cap.
Know Services Affected
The reporting and collection requirements of beneficiary functional data apply to all claims for services furnished under the Medicare Part B outpatient therapy benefit and the PT, OT, and SLP services furnished under the Comprehensive Outpatient Rehabilitation Facility (CORF) benefit, clarified MLN Matters® article number MM8005 which was updated by Change Request Number: 8005.
“They also apply to the therapy services furnished incident to the service of a physician and certain Non-Physician Practitioners (NPPs), including, as applicable, Nurse Practitioners (NPs), Certified Nurse Specialists (CNSs), and Physician Assistants (PAs),” CMS says.
When To Use “Other” Category
If your patient’s functional limitation does not fit into one of the predefined categories, you can use the “other” category.
Those who use tools like FOTO can report composite functional scores by using G8990, G8991, and G8992, according to the APTA. If the patient achieves his goal and there is a second condition, you should use the G-codes G8993-G8896 for “other subsequent” functional limitation.
Remember to contact your billing service or billing software vendor to ensure they can properly process these G-codes now they have gone into effect.
Resource: See www.cms.hhs.gov/manuals.
Editor’s note: For more on G-code guidelines, see Eli’s Rehab Report, Vol. 20, No. 7.